Case Report
Braganza Adrian*, MS, Aarti Heda, DNB, Varun Kharbanda, MS, and Rohit Shetty, DNB
Department of Cataract And Refractive Surgery, Narayana Nethralaya Post-Graduate Institute of Ophthalmology, Bangalore, India
Corresponding author
Braganza Adrian, Narayana Nethralaya Health city (Narayana Hrudayalaya Campus), #258/A, Bommasandra, Hosur Road, Bangalore ? 560099, India, Tel: +91-9945149518; E-mail: dradrianbraganza@gmail.com
Received Date: 29th January 2015
Accepted Date: 11th February 2015
Published Date: 16th February 2015
Citation
Braganza A, Heda A, Kharbanda V, Shetty R (2015) Topiramate Induced Bilateral Simultaneous Angle Closure Glaucoma in A Steroid Responder. Enliven: Clin Ophthalmol Res 1(1): 003.
Copyright
@ 2015 Dr. Braganza Adrian. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
To report a case of topiramate induced bilateral simultaneous angle closure glaucoma in a young male patient who also developed steroid response following conventional treatment ie, cessation of the causative drug (Topiramate),topical and oral steroids along with antiglaucoma medication. There was an initial drop in Intra-ocular Pressure (IOP) subsequently followed by a secondary rise in IOP due to steroid response despite the resolution of topiramate induced bilateral ciliochoroidal effusions.
Keywords
Topiramate; Bilateral angle closure glaucoma; Steroid responder
Introduction
Topiramate is an oral sulfamate medication used primarily for epilepsy and migraine [1]. The doses used commonly are in the range of 50 mg - 400 mg per day. In the ?certain? category of the World Health Organisation classification system, adverse ocular side effects associated with topiramate include abnormal vision, acute IOP elevation, acute myopia, diplopia, nystagmus and shallow anterior chamber with angle-closure [2]. Prompt cessation of therapy alone can result in rapid resolution of most of these adverse effects, whereas, failure to recognise these ocular side effects can lead to permanent visual problems [3]. Ophthalmologists should be aware of the documented side effects of topiramate, particularly when presented with simultaneous bilateral acute angle-closure glaucoma. Neurologists initiating therapy with topiramate should also educate the patients of its potential side effects and importance of reporting back immediately in case of any visual disturbances.
Prompt cessation of topiramate is the mainstay of treatment. Supportive treatment in the form of oral and topical antiglaucoma drugs to reduce the intraocular pressure, topical steroids to bring down the inflammation, and topical cycloplegics to retract the ciliary processes thus bringing down the intraocular pressure has been recommended [4]. However, care should be taken while treating patients with topical steroids because persistent raised intraocular pressure as a steroid response could be misdiagnosed as non-resolution of symptoms and present the clinician with dilemma.
We report a case of topiramate induced angle closure glaucoma who being a steroid responder continued to have high intraocular pressure despite stopping topiramate and starting treatment with topical steroids, which is one of the documented treatments for this form of glaucoma.
Case History
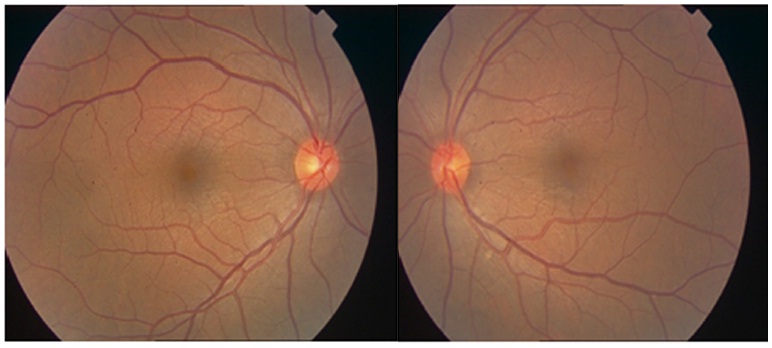
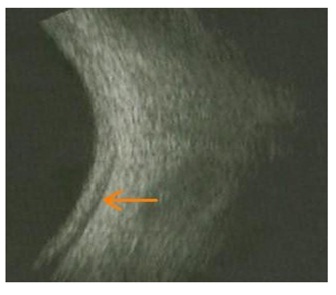
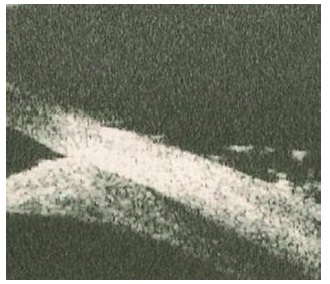
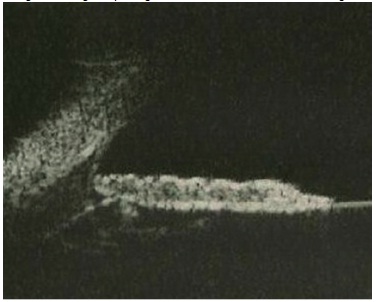
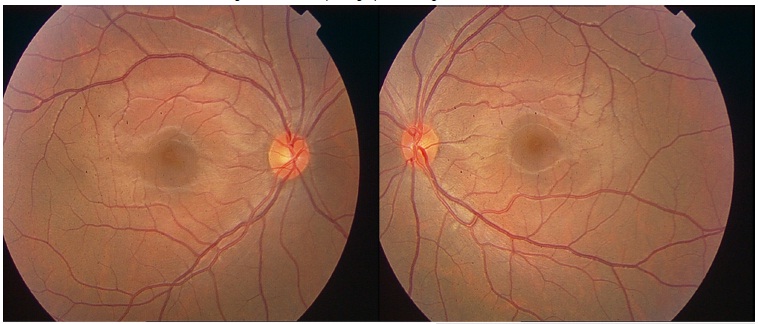
A Nineteen year old male patient presented with complaints of sudden onset of blurring of distance vision of one day duration. He was a known case of simple myopia and was using glasses for distance since one year and was comfortable with his glasses till one day before presentation. He had a history of migraine and was on treatment for it on and off. He had been started on Topiramate Tablet 50 mg by the neurologist for migraine one week back. Unaided visual acuity at presentation was recorded as 3/60, N6 both eyes. Patient?s own glass power was -0.50 DSph and -0.75 DSph in right and left eyes respectively. His best corrected visual acuity was 6/6, N6 both eyes with -6.50 DSph. Anterior segment examinations showed a shallow anterior chamber (Van Herick's Grade II). Rest of the anterior segment findings were within normal limits. Intraocular pressure was 40 and 42 mm Hg by applanation tonometry in right and left eyes respectively. Gonioscopy showed closed angles in both eyes. Fundus examination showed a cup-disc ratio of 0.2:1 and internal limiting membrane folds at the macula in both eyes (Figure1). B-scan ultrasound showed choroidal effusions in both eyes (Figure 2). Ultrasound biomicroscopy showed closed angles with anterior shift of iris-lens diaphragm and confirmed the presence of choroidal effusion (Figure 3). Based on the above findings, a diagnosis of Topiramate induced acute angle closure glaucoma was made and patient was advised to stop Topiramate immediately. In addition, he was started on oral carbonic anhydrase inhibitors (Acetazolamide 250 mg) 3 times a day, topical beta-blockers and ? agonist combination eyedrops both eyes twice daily, topical cycloplegics eyedrops both eyes twice daily, topical steroids (Prednisolone acetate eyedrops) both eyes six times a day and systemic steroids ie Tab Prednisolone 40 mg once daily. Three days after the onset of treatment, visual acuity was recorded as 6/9, N6 both eyes with patient?s own glasses. Intraocular pressure was recorded as 16 mm Hg in both eyes. Ultrasound biomicroscopy showed deepening of anterior chamber and decrease in choroidal effusion (Figure 4). Fundus examination showed resolution of internal limiting folds (Figure 5). At this visit, systemic steroids were tapered (20 mg once daily x 4 days and stop), topical steroids were tapered on weekly basis and stopped, topical beta blockers and cycloplegics were stopped simultaneously and he was advised to stop oral carbonic anhydrase inhibitors after 3 days. One week after stopping all antiglaucoma medications, his intraocular pressure was recorded as 20 and 18 mm Hg in right and left eyes respectively. On the follow up visit two weeks after stopping the antiglaucoma medications, his visual acuity was recorded as 6/6, N6 with his glasses. But intraocular pressure was recorded as 33 and 30 mm Hg in right and left eyes respectively. Gonioscopy showed open angles, B-scan showed resolving choroidal effusion. Based on the findings of initial reduction of intraocular pressure with antiglaucoma medications and a repeat rise in intraocular pressure while continuing steroid treatment, he was suspected to be a steroid responder and was advised to stop topical steroids and was restarted on systemic carbonic anhydrase inhibitors. Three days after stopping topical steroids, intraocular pressure was recorded as 8 mm Hg in both eyes. At this visit he was advised to stop systemic carbonic anhydrase inhibitors. Two weeks after stopping all medications, his intraocular pressure was recorded as 16 mm Hg in both eyes. Visual field examination done at this visit was within normal limits in both eyes.
Figure 1: Fundus photograph at presentation showing ILM folds at the macula in both eyes
Figure 2: B-scan image showing choroidal effusion
Figure 3: UBM image showing choroidal effusion
Figure 4: UBM image showing deepening of anterior chamber and resolving choroidal effusion
Figure 5: Fundus photograph showing resolved ILM folds
Discussion
Topiramate is a sulfamate-substituted monosaccharide and is prescribed for various disorders such as seizures, infantile spasms, neurophthalmic migraine, and depression, and also off-label for bipolar disorders and as a weight reducing agent5. The precise mechanism of its action is unknown. It has a weak inhibitory action on some of the iso enzymes of carbonic anhydrase.
Topiramate was first implicated as a cause of bilateral acute angle closure glaucoma in a case report by Banta et al. [6] in July, 2001. The basic mechanism underlying drug-induced acute myopia with topiramate seems to be ciliary effusion causing ante-version of the ciliary body and anterior displacement of the iris-lens diaphragm. This induces bilateral acute myopia, non pupillary block angle closure, and raised IOP [7].
Topiramate induced angle closure is an indiosyncratic reaction and can occur in otherwise normal eyes with normal anterior chamber angles. Ocular examination before starting topiramate cannot identify eyes at risk [8]. Identification of cause by taking a detailed history including the drug history can lead to an accurate diagnosis and prompt treatment. Suspicion of drug induced acute angle closure glaucoma should be high when it presents bilaterally simultaneously in a young individual.
Corticosteroid-induced elevation of IOP in susceptible patients as a result of reduced outflow, is possible with topical, other local (dermal or inhalational, for example), depot (subconjunctival, sub-Tenon?s and intravitreal), or systemic steroid preparations [9]. Theories that have been postulated to result in the elevated intraocular pressure associated with steroid application include inhibition of catabolic enzymes due to stabilization of lysosomal membranes resulting in accumulation of glycosaminoglycans [10] and decreased synthesis of prostaglandins that regulate aqueous humour outflow [11]. Most patients who respond to topical steroids will develop an elevation within six weeks to two months and once the topical steroids have been ceased, the IOP almost always returns to baseline within 4 weeks [9].
A close observation of the patient during treatment and maintaining high degree of suspicion is important in the treatment of topiramate induced angle closure glaucoma. Our patient responded to the initial treatment with antiglaucoma medications and maintained the reduction in intraocular pressure even after stopping the antiglaucoma treatment for one week. The intraocular pressure increased after two weeks of treatment with topical steroids which is classical time for patients to present with steroid response. Repeat ultrasound biomicroscopy and B- scan in our patient revealed that the underlying cause of secondary closure, ie. ciliochoroidal effusions was subsiding, which helped us to identify steroid-response as the cause of persistent high intraocular pressure. To our knowledge, there is no previous report of topiramate induced glaucoma in a steroid repsonder.
Summary
Topical steroids are a part of treatment for angle closure induced by Topiramate. There are no reports that show topiramate induced bilateral angle closure episode in a steroid responder. This case presents the challenges faced by the clinician and their management in such a situation.
References
- Silberstein SD, Dodick DW, Lindblad AS, Holroyd K, Harrington M, et al. (2012) Randomized, placebo-controlled trial of propranolol added to topiramate in chronic migraine. Neurology 78: 976-984.
- Fraunfelder FW, Fraunfelder FT (2004) Adverse ocular drug reactions recently identified by the National Registry of Drug-Induced Ocular Side Effects. Ophthalmology 111: 1275-1279.
- Sachi D, Vijaya L (2006) Topiramate induced secondary angle closure glaucoma. J Postgrad Med 52: 72-73.
- Fraunfelder FW, Fraunfelder FT, Keates EU (2004) Topiramate-associated acute, bilateral, secondary angle-closure glaucoma. Ophthalmology 111: 109-111.
- Raritan NJ (2001) Topomax. Ortho-McNeil Pharmaceutical Inc.
- Banta JT, Hoffman K, Budenz DL, Ceballos E, Greenfield DS (2001) Presumed topiramate induced bilateral acute angle closure glaucoma. Am J Ophthalmol132: 112-114.
- Spaccapelo L, Leschiutta S, Aurea C, Ferrari A (2009) Topiramate-associated acute glaucoma in a migraine patient receiving concomitant citalopram therapy: A case-report. Cases J 2: 87.
- Levy J, Yagev R, Petrova A, Lifshitz T (2006) Topiramate-induced bilateral angle-closure glaucoma. Can J Ophthalmol 41: 221-225.
- Peyman GA, Sanders DR, Goldberg MF (1987) Principles and Practice of Ophthalmology. 1st Indian Edition, 1: 708.
- Armaly MF (1963) Effect of corticosteroids on intraocular pressure and fluid dynamics: the effect of dexamthasone in the normal eye. Arch ophthalmol 70: 482.
- Weinreb RN, Mitchell ME, Polansky JR (1983) Prostaglandin production by human trabecular cells: in vivo inhibition by dexamethasone. Invest Ophthalmol Vis Sci 24: 1541-1545.