Case Report
Gohar Mushtaq1*, Shahzad Khan2, Iqbal Hussain3, and Mohammad A. Kamal4
1Department of Biochemistry, College of Science, King Abdulaziz University, Jeddah, Saudi Arabia
2Wuhan University School of Medicine, Wuhan 430071, Hubei, China
3Department of Critical Care Medicine, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia
4King Fahd Medical Research Center, King Abdulaziz University, P. O. Box 80216, Jeddah 21589, Saudi Arabia
Corresponding author
Gohar Mushtaq, Department of Biochemistry, College of Science, King Abdulaziz University, Jeddah, Saudi Arabia; E-mail: gmushtaq2000@yahoo.com
Received Date: 23rd July 2015
Accepted Date: 05th October 2015
Published Date: 09th October 2015
Citation
Mushtaq G, Khan S, Hussain I, Kamal MA (2015) Schwannoma of Lumbar Spine: A Medical Case Study. Enliven: Neurol Neurotech 1(1): 001.
Copyright
@ 2015 Dr. Gohar Mushtaq. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, that permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Schwannomas refer to benign, encapsulated tumors that derive from the nerve sheath. This report presents the case of a 53 year old patient with chronic
back pain which was initially misdiagnosed as unilateral meningoceles but, later on, MRI scan with contrast disclosed the presence of lumbosacral
schwannoma which appeared as solid heterogeneous lesion which would lie within and expand the left neural exit foramen, extending into the
paravertebral soft issues with marked mass effect on the adjacent psoas muscle. Instead of surgically removing the schwannoma, musculoskeletal
imaging guided nerve root injection of corticosteroid was administered to the patient as a palliative treatment. Clinical and radiological features of this
rare and often misdiagnosed medical finding will be accentuated in this case report and treatment strategy will be discussed.
Keywords
Schwannoma; Tumors; Low back pain; Lumbosacral; Nerve root; Spine; Nerve root injection
Introduction
Schwannomas refer to benign, encapsulated tumors of the nerve sheath. They originate from the myelin-producing Schwann cells of the nervous system and are usually well encapsulated with a distinctive histologic pattern. Neurilemmoma is a synonymous term to schwannoma. Schwannomas are uncommon and comprise of around 3% of all spinal tumors [1]. Symptoms of schwannomas of the lumbar spine are usually vague (similar to a compressive neuropathy) and it may take months to years before establishing the diagnosis. The most common clinical manifestations of spinal schwannomas include back pain, sciatica, fatigue, and weakness or numbness in the arms and legs [2,3].
Schwannomas are sometimes confused with neurofibromas due to their similar appearance although the two conditions are quite different. Neurofibromas are hard to remove surgically due to the ability of neurofibratomas to penetrate deep into the nerve root and become part of it. Thus, surgical removal of neurofibromas almost always results in damaging the nerve itself and neurological deficits [4]. On the other hand, schwannomas do not penetrate into the nerve root and only press against the fascicular groups without causing any damage. Therefore, schwannomas can usually be removed without causing neurological deficits [5,6]. Without high-resolution imaging techniques (such as CT scan, MRI scan), it is easy to miss the cases of lumbosacral schwannomas and misdiagnose them as lumbar (intervertebral) disk disease. This happens due to high number of cases with typical clinical presentation of a disc disease encountered by physicians among their patients. This report presents the case of a 53 year old patient with chronic back pain which was initially misdiagnosed as unilateral meningoceles but, later on, MRI scan with contrast disclosed the presence of lumbosacral schwannoma as it shall be discussed in detail in this report.
Case Report
Here we are presenting the case of a male patient in his early 50?s, which was brought to our attention because of the occurrence of schwannoma of lumbar spine. At the age of 47 years, he started suffering from frequent, high-grade back pain with associated neuralgia in the legs. The patient manifested no clinical signs of neurological deterioration while his sensorimotor functions remained intact. The patient also showed no signs of impaired bowel/bladder functions. However, the patient complained of marked lower back and knee pain in muscles and bones, dyspnea upon exertion and chronic fatigue. Based on the preliminary clinical assessment, the patient was diagnosed with lumbar degenerative disk disease. In order to further investigate the condition, a computerized tomography scan (CT scan) of the lower part of the spine, that is, the lumber region and the sacrum, was performed on the patient from T12 to the middle of the sacral region. An initial CT scan imaging of the patient revealed the presence of homogeneous and distinct masses located on the spinal column and raised the possibility of the presence of unilateral meningoceles with canal stenosis [7]. Furthermore, no evidence of instability was identified within the cervical or lumbar spine on flexion and extension. Vertebral body and intervertebral disc heights were preserved. No focal bone lesion was noticed and the disc space heights appeared within normal range as revealed by CT scan imaging. The patient was put on symptomatic treatment which included restriction of heavy weights, frequent bed rest and over-the-counter analgesics (non-steroidal anti-inflammatory drugs). However, no improvement in patient?s symptoms was noted the 6-weeks period follow-up visit. At that stage, magnetic resonance imaging (MRI) with contrast was suggested to be performed.
In the MRI of the cervical spine, the following sequences had been obtained ? axial T1, T2 and STIR axial T2: sagittal oblique T2. The MRI scan revealed that alignment of the cervical spine was satisfactory with the patient in a supine position. No signal abnormality within the cervical or visualized upper thoracic cord was recorded. At C2/3, there was mild loss of intervertebral disc height posteriorly. No intervertebral disc bulge or prolapse was identified. There was no central canal or neural exit foraminal stenosis and no significant facet joint arthropathy. At C3/4 and C4/5, there was no intervertebral disc height posteriorly. There was no central canal or neural exit foraminal stenosis. No significant facet joint arthropathy was noticed. At C5/6, there was a mild diffuse disc bulge without evidence of central canal or neural exit foraminal stenosis but no significant facet joint arthropathy. Also, there was no lesion/abnormality of the paravertebral soft tissues. Normal flow voids were demonstrated within the carotid and vertebral arteries within the neck.
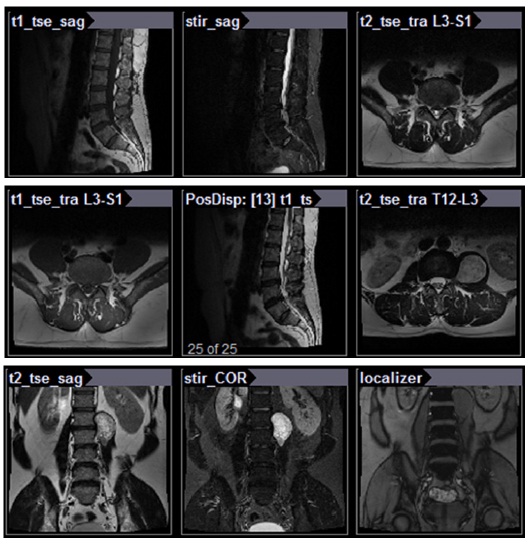
In the MRI of the lumbar spine, the following sequences had been obtained ? sagittal T1, T2 and STIR: axial T1 and T2. Intravenous Gadolinium was then administered and 3-plane T1FS sequences were obtained. The findings were as follows: The vertebral bodies had been numbered with the least major disc space to represent L5/S1. The conus would terminate normally at the level of T12. Alignment of the lower thoracic and lumbar spine appeared satisfactory. Partial sacralisation of the L5 vertebral body was also noted (Figure 1). More importantly, there was a solid heterogeneous enhancing mass lesion which arose from and caused widening of the left neural exit foramen at L1/2, measuring 30 x 48 x 60mm in AP, transverse and superior/inferior dimensions. There was marked mass effect on the adjacent psoas muscle without frank invasion. Given the characteristics and location of that lesion, it most likely represents a schwannoma. Furthermore, from T10/11 to L1/2, no intervertebral disc bulge or prolapse was identified. There is no central canal or neural exit foraminal stenosis. At L2/3, there was a left foraminal/far lateral disc protrusion which would touch the exiting L2 nerve root and may cause irritation. There was no central canal or right neural exit foraminal stenosis. No significant facet joint arthropathy was noted. At L3/4, there was moderate diffuse disc protrusion which would abut both left and right L4 nerve roots within their respective lateral recesses, greatest on the left. No significant neural exit foraminal stenosis and facet joint artropathy was identified. There was moderate canal stenosis. At L5/S1, there was no intervertebral disc bulge or prolapsed with no central canal or neural exit foraminal stenosis.
Figure 1: Lumbar spine magnetic resonance imaging scans showing the presence of a schwannoma
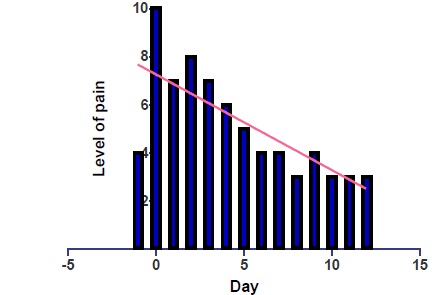
Instead of surgically removing the schwannoma, the patient was given palliative treatment in the form of corticosteroid injection into the facet joints. Informed consent was obtained and sterile field was established. 2mL of 2% Xylocaine (local anesthetic) was introduced into the overlying soft tissue. A 23-guage needle was then introduced into the neural exit foramina of the left L5 and left S1 nerve roots under CT guidance. Extravascular and extradural position was confirmed with contrast. One ampoule of Celestone (corticosteroid), 1 mL of 2% Xylocaine and 1mL of 0.5% Marcaine (local anesthetic) was injected. To evaluate the efficacy of the corticosteroid injection, the patient?s condition was assessed in the follow up visits with respect to scale of pain severity, back mobility and ability to freely move. In order to determine if the injection had been effective, the patient was asked to keep a record of his pain levels immediately post injection and for the next 12 days, reporting the degree of pain from a scale of 0 (no pain) to 10 (extreme pain). The patient tolerated the procedure extremely well, reporting pain reduction from 10/10 to 3/10 (Figure 2). No immediate post-procedure complication was encountered. The patient was followed up for 6 months and will continue to be followed semiannually.
Figure 2: The patient?s level of pain each day from immediately post injection and for the next 12 days
Discussion
This report presents one of the rare types of schwannoma, i.e. lumbosacral schwannoma. This rare type of benign tumor resembled lumbar degenerative disk disease and gave the misimpression of a lateral meningocele upon CT scan. Finally, MRI scan with contrast helped us in the diagnosis of our patient who remained undiagnosed and was suffering from persistent back pain for years as a result of schwannoma in the lumbosacral spine. Contrast MRI helps in accurate diagnosis of schwannomas because these solid benign tumors appear well-enhanced compared to other lesions that usually lack such structure [8]. MRI scans provide high contrast resolution and multiplanar capabilities, thereby identifying and characterizing the lesions in a non-invasive manner [9]. MRI findings revealed the presence of solid heterogeneous lesion which lies within and expands the left neural exit foramen at L1/2, measuring 30 x 48 x 60mm, extending into the paravertebral soft issues with marked mass effect on the adjacent psoas muscle. Given the location and the MRI appearance of this lesion, it most likely represents a schwannoma. Most of the times, schwannomas may manifest only in the form of back pain or partial paralysis of the lower limbs in otherwise asymptomatic patients and cannot be usually diagnosed based on clinical exam alone. Performing MRI scan with contrast aids in the accurate diagnosis of this condition even though a final histopathological exam would provide a definitive identification [10]. In general, T1-weighted images of schwannomas appear as hypointense or isointense while T2-weighted images appear as hyperintense on MRI scans. After intravenous administration, gadolinium enhancement is mostly homogeneous [11].
Controversy surrounds regarding what approach to take in treating schwannomas [12]. Some physicians and surgeons recommend complete excision of schwannomas which would also involve sacrificing the nerve root. Although there are usually good results from surgical treatment of schwannomas of lumbar spine, there are chances (less than 15%) of postoperative neurological deficits due to spinal surgical trauma [13,14]. Post-surgical neurological deficits, mostly attributed to the contusion of the remaining continuous nerve fibers, may last as a neurological disability lasting for several months to few years [15]. In addition, there is always a rare possibility of tumor recurrence in some patients especially in cases of inadequate removal of the tumor, thereby necessitating repeat surgeries [16,17]. Hence, musculoskeletal imaging guided nerve root injection of corticosteroid was administered to the patient. The patient reported more improvement, less pain and less physical disability on 3 month and 6 month follow-up visits. There will be long term clinical and radiographic follow up for this patient. To sum up, this rare finding may be useful for surgeons and physicians in the accurate diagnosis of patients with chronic back pain with or without accompanying symptoms of lumbosacral schwannoma and they may utilize effective treatment strategies for the patients.
Acknowledgments
The authors would like to thank the facilities provided by the Department of Biochemistry, College of Science and the KFMRC, King Abdulaziz University, Jeddah, Saudi Arabia, the Department of Critical Care Medicine, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia as well as the LC/MS Metabolite Identification Division of Metabolomics at Buena Park, California, USA. The authors are grateful to Dr. Charles New for performing MRI scan of the lumbosacral spine on the patient. The authors also owe a debt of gratitude to the relatives of the patient for their cooperation throughout the course of this study.
Conflict of Interest Statement
The authors confirm that this article content has no conflict of interest.
References
- Chick G, Alnot JY, Silbermann-Hoffman O (2000) Benign solitary tumors of the peripheral nerves. Rev Chir Orthop Reparatrice Appar Mot 86: 825-834.
- Dubuisson A, Fissette J, Vivario M, Reznik M, Stevenaert A (1991) A benign tumor of the sciatic nerve: Case report and review of the literature. Acta Neurol Belg 91: 5-11.
- Chiang ER, Chang MC, Chen TH (2009) Giant retroperitoneal schwannoma from the fifth lumbar nerve root with vertebral body osteolysis: A case report and literature review. Arch Orthop Trauma Surg 129: 495-499.
- Burns SH, Thiel HW, Cassidy JD, Kirkaldy-Willis WH (1989) Nerve-root Schwannomas mimicking intervertebral disc herniations: a report of two cases. J Can Chiropr Assoc 33: 135-141.
- Jinnai T, Koyama T (2005) Clinical characteristics of spinal nerve sheath tumors: Analysis of 149 cases. Neurosurgery 56: 510-515.
- Kehoe NJ, Reid RP, Semple JC (1995) Solitary benign peripheral nerve tumours. Review of 32 years? experience. J Bone Joint Surg 77: 497-500.
- Mushtaq G, Hussain I, Khan JA, Kamal MA (2015) Lateral meningocele syndrome with asymmetric canal stenosis: A case study. Saudi J Biol Sci 22: 102-105.
- Turgut M, Erku? M (2008) Giant schwannoma of the cauda equina: case report and review of the literature. Zentralbl Neurochir 69: 99-101.
- Katonis P, Kontakis G, Pasku D, Tzermiadianos M, Tzanakakis G, et al. (2008) Intradural tumours of the lumbar spine presenting with low back pain: report of two cases and review of the literature. Acta Orthop Belg 74: 282-288.
- Rustagi T, Badve S, Parekh AN (2012) Sciatica from a foraminal lumbar root schwannoma: Case report and review of literature. Case Rep Orthop 2012: 142-143.
- Hems TE, Burge PD, Wilson DJ (1997) The role of magnetic resonance imaging in the management of peripheral nerve tumours. J Hand Surg Br 22: 57-60.
- Kagaya H, Abe E, Sato K, Shimada Y, Kimura A (2000) Giant cauda equine Schwannoma. A case report. Spine (Phila Pa 1976) 2: 268-272.
- Lu DC, Dhall SS, Mummaneni PV (2009) Mini-open removal of extradural foraminal tumors of the lumbar spine. J Neurosurg Spine 10: 46-50.
- Russell SM (2007) Preserve the nerve: Microsurgical resection of peripheral nerve sheath tumors. Neurosurgery 61: 113-118.
- Karekezi C, Egu K, Djoubairou BO, Boutarbouch M, Ouahabi AE (2014) Unusual cause of non-discogenic sciatica: Foraminal lumbar root schwannoma. Surg Neurol Int 5: S208-S210.
- Vadivelu S, Prasad P, Adesina AM, Kim E, Luerssen TG, et al. (2013) Giant invasive spinal schwannoma in children: a case report and review of the literature. J Med Case Rep 7: 289.
- Santi MD, Mitsunaga MM, Lockett JL (1993) Total sacrectomy for a giant sacral schwannoma. A case report. Clin Orthop Relat Res 294: 285-289.