Research Article
Selma Freire Carvalho Cunhasup*1, Mariana Pietrobom Pupin2, Daiane Leite da Roza3, Mariana Guimarães2, Larissa Angélica Possebom Dela Marta2, Rafaela Monte Alegre2, Eduardo Ferrioli4, and Julio Sergio Marchini1
1 Division of Clinical Nutrition, Department of Internal Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil
2 Dietitian from Clinical Hospital, School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil
3 Department of Social Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil
Division of Geriatrics, Department of Internal Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil
Corresponding author
Selma Freire Carvalho Cunha, Division of Clinical Nutrition, Department of Internal Medicine, School of Medicine of Ribeirão Preto, University of São Paulo, Ribeirão Preto, Brazil, E-mail: sfreire@fmrp.usp.br
Received Date: 17th December 2016
Accepted Date: 15th March 2017
Published Date: 25th March 2017
Citation
Cunha SF, Pupin MP, Roza DL, Guimarães MP, Dela Marta LAP (2017) Nutritional Risk and Malnutrition in Elderly Patients’recently Hospitalized. Enliven: J Diet Res Nutr 4(1): 002.
@ 2017 Dr. Selma Freire Carvalho Cunha. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction:
High prevalence of malnutrition in the growing population of older adults makes nutritional screening mandatory for hospitalized elderly patients.
Objective:
Identify nutrition risk and the odds ratio of nutritional screening data of elderly (≥ 65 years old) to adult (21 to 64 years old) patients recently admitted to a tertiary hospital.
Casuistic and Methods:
We applied the Subjective Global Assessment (SGA) protocol in 2478 patients within 48 hours after admission to a public hospital. Subjects were divided into Elderly Group (n = 733) and Non-elderly Group (n = 1745). The data were submitted to Chi-Square test. The quantification of this association was measured using logistic regression models.
Results:
Elderly patients showed a high percentage of nutritional risk or mild/moderately malnourished (41 vs. 32%). The prevalence of severe malnourished was similar between the study groups (10 vs. 9%).
Results of logistic regression showed the odds ratio (OR) of elderly patients were greater for weight loss (OR=1.30), in quantity (OR=1.29) and consistency of food (OR=1.85) changes in the pattern of food intake, anorexia (OR=1.69) and dysphagia (OR=1.56), when compared to the adults. Besides that, elderly patients presented greater risk of diseases with increased metabolic demand and clinical signs of nutritional deficiencies.
Conclusions:
Prevalence of nutritional risk and malnutrition was high in the patients evaluated, and elderly subjects showed higher nutritional risk when compared to other hospitalized patients.These results can be attributed to changes in the pattern of food intake due to anorexia and dysphagia, associated with higher prevalence of diseases with increased metabolic demand.
Keywords
Nutritional screening; Malnutrition; Subjective global assessment; Hospital setting; Elderly
Introduction
Seniors are the fastest growing population worldwide and they use more hospital services than other age groups. Their treatment has a longer duration and a slower recovery, which causes higher costs [1]. Besides, elderly patients present debilitated nutritional status that result in poor quality of life, increased adverse reactions to medications, inadequate response to treatment and worse prognosis [2].
Therefore, high prevalence of malnutritionin older adult population makes nutritional screening necessary for hospitalized elderly patients. Nutritional risk has been documented in about 50% hospitalized geriatric patients or more [3-6]. Subjective Global Assessment (SGA) [7] has been used as a nutritional screening tool in hospitalized patients [8] because it is simple, non-invasive and inexpensive. A study using the SGA conducted with 4000 hospitalized patients in Brazil showed nutritional risk was higher in the elderly (53%) when compared to the non-elderly (45%) [9].
The hypothesis of this study was the high prevalence of nutritional risk and malnutrition in the elderly compared to the non-elderly. In this context, the objective was to compare the nutritional risk of elderly to non-elderly patients recently hospitalized, and identify the risk factors that influence the nutritional classification by SGA.
Casuistic and Methods
This retrospective study was conducted in a tertiary university hospital, after approval by the Institutional Ethics Committee (Protocol #13530). The initial casuistic included data from nutritional screening of 3450 recently hospitalized patients (<48 hours after admittance), excluding those in the Pediatric, Psychiatry, Obstetrics/Gynecology wards and Intensive Care Unit. The final casuistic comprised 2478 patients from different wards after excluding misleading cases or with incomplete information (n = 442) and patients younger than 21 years old (n=530). We classified the subjects to age; patients over 65 years old were allocated to the Elderly Group (n = 733, 73 ± 6 years, 57% male) and those under 64 years old integrated the Non-elderly Group (n = 1745, 46 ± 12 years, 50% male).
Previous body weight (six months prior hospitalization) and current body weight were documented and the change during this period was calculated. Unintentional reduction in food intake was determined, besides consumption of liquid and semi-liquid food with lower energy density. We documented the occurrence of gastrointestinal symptoms longer than two weeks and alterations in functionalphysical capacityin relation to habitual. The clinical diagnoses were obtained from patients’ health records, and the degree of metabolic stress was determined. According to SGA protocol, a simplified physical exam was performed to identify clinical manifestations of malnutrition (edema, loss of subcutaneous fat, skin desquamation and angular cheilosis. The dorsum and lateral margins of the outer surface of the tongue were inspected, in order to identify atrophic alterations in the tongue papillary. Papillary atrophy wasdiagnosed when observed a flattening mucosa in the tip and lateral borders of the tongue, giving this organ a smooth, slick aspect.
All data were collected by trained dieticians and individual information was revised by one independent dietician and one physician specialized in clinical nutrition. According to SGA criteria, the subjects were classified as well nourished, moderately (or suspected of being) malnourished or severely malnourished.
To verify the association between the qualitative variables, the data were submitted to Chi-Square test. In addition, the quantification of this association was measured by logistic regression models [10], where the gross Odds Ratio (OR) was calculated with its respective 95% confidence intervals (95%CI). All statistical analyzes were performed using statistical software SAS (SAS Institute Inc., SAS/STAT® User’s Guide, Version 9, Cary, NC: SAS Institute Inc., 2002). Values of p less than 0.05 were considered significant.
Results
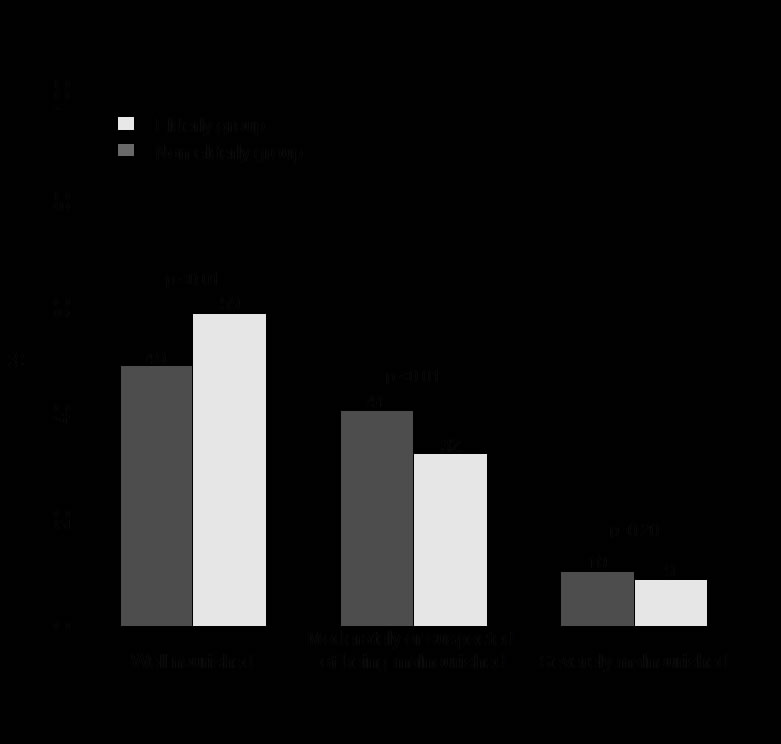
According to the nutritional classification of GSA protocol [7], elderly patients recently hospitalized presented a higher prevalence of moderately or suspected of being malnourished when compared to those non-elderly (Figure 1).
Figure 1. Nutritional classification according to the Subjective Global Assessment (SGA) in elderly (n = 733, ?65 years old) and non-elderly patients (n = 1745, 21-64 years old) recently hospitalized(<48 hours after admittance).
Elderly patients (Table 1) had increased odds of weight loss [OR=1.30 (1.08; 1.56)], anorexia [OR=1.69 (1.35; 2.13)], dysphagia [OR=1.56 (1.16; 2.09)], reduction of food intake [OR=1.29 (1.07;1.54)] and ingestion of liquid and semi-liquid food [OR=1.85 (1.41; 2.43)]. Compared with non-elderly subjects, the elderly group presented greater odds of carrying diseases that cause inflammatory stress [OR=1.35 (1.12; 1.63)], and theyhad an increased odds of reduction in functional capacity. Elderly patients had higher odds of presenting clinical manifestations of nutritional deficiencies such as edema [OR=1.40 (1.14; 1.72)], loss of subcutaneous fat [OR=2.28 (1.83; 1.85)], flaking skin [OR=1.49 (1.11; 2.00) and papillary atrophy of the tongue (OR=1.57 (1.30; 1.90)].
| Elderly group (n=733) | Non-elderly group (n=1745) | p value | ||
| Weight change | ||||
| Weight 6 months prior to study (kg) | 69 ±14 | 74 ± 19 | < 0.01 | |
| Current weight (kg) | 66 ±14 | 72 ± 19 | < 0.01 | |
| Patients who lost weight [% (n)] | 59 (378) | 51 (847) | 0.004 | |
| Lostweightwithin6months (%) | 10 ± 7 | 10 ± 8 | 0.53 | |
| Change in food intake | ||||
| Reduction of food intake [% (n)] | 36 (263) | 30 (529) | 0.06 | |
| Liquid and semi-liquid food [% (n)] | 14 (102) | 8 (140) | <0.001 | |
| Gastrointestinal symptoms | ||||
| Anorexia [% (n] | 21 (150) | 13 (230) | <0.001 | |
Abdominal distension[% (n)] |
10 (75) | 10 (178) | 0.98 | |
| Abdominal pain [% (n)] | 8 (56) | 7 (122) | 0.56 | |
| Nausea [% (n)] | 16 (118) | 15 (248) | 0.40 | |
| Vomiting [% (n)] | 6 (47) | 7 (120) | 0.68 | |
Dysphagia[% (n)] |
11 (80) | 7 (127) | 0.003 | |
| Diarrhea [% (n)] | 7 (50) | 6 (105) | 0.45 | |
| Functional capacity | ||||
| No dysfunction [% (n)] | 58 (428) | 70 (1220) | < 0.001 | |
| Working suboptimally [% (n)] | 32 (233) | 23 (393) | < 0.001 | |
| Just walk[% (n)] | 6 (44) | 5 (79) | < 0.001 | |
| Bedridden [% (n)] | 4 (28) | 3 (52) | < 0.001 | |
| Disease and its relation to nutritional needs | ||||
| Inflammatory stress [% (n)] | 33 (239) | 26 (460) | 0.002 | |
| Physical examination data | ||||
| Edema [% (n)] | 74 (541) | 80 (1394) | <0.001 | |
| Loss of subcutaneous fat [% (n)] | 25 (182) | 13 (220) | <0.001 | |
| Hair loss [% (n)] | 15 (120) | 21 (361) | 0.01 | |
| Change in hair color[% (n)] | 1 (3) | 1 (12) | 0.41 | |
| Flakingskin[% (n)] | 11 (80) | 8 (132) | 0.007 | |
| Papillary atrophy of the tongue [% (n)] | 34 (249) | 25 (431) | <0.001 | |
| Angular cheilosis [% (n)] | 1 (11) | 2 (22) | 0.85 | |
| Pressure injury [% (n)] | 1 (6) | 1 (16) | 0.81 | |
Table 1. Data of the various items of Subjective Global Assessment in elderly ( =or>65 years old) and non-elderly patients (21-64 years old) recentlyhospitalized (<48 hours after admittance).
Discussion
This work showed that newly admitted elderly patients in a tertiary hospital presented a higher prevalence of moderately or suspected of being malnourished when compared to non-elderly patients. Theprevalence of severe malnutrition was similar between the study groups, given the severity of clinical conditions and regardless the patients’ age.
Compared with the non-elderly, the elderly patients showed an increased chance of loss of weight and subcutaneous tissue, indicating that the adipose reserve is lower in old adults [11]. However, evidence suggests weight loss in the elderly occurs mainly due to depletion of lean body mass, which limits activities of daily living [12]. In our study, anorexia was common in hospitalized elderly patients, similar to the prevalence observed in institutionalized elderly [13]. This condition can be related to the co-morbidity that led to hospitalization or the effects of aging [14]. Anorexia represents a predictive factor for mortality in hospitalized and institutionalized subjects [15]. Reduction in food intake and intake of liquid and the semi-liquid food were more common in the elderly than non-elderly patients. In Spain, 81% of 2834 institutionalized elderly subjects changed the consistency of food, and 43% had dysphagia [16]. The elderly presented the higher risk of dysphagia [17], which may contribute to poor nutritional status and lead to malnutrition if not identified [18]. Among dependent older adults, 59% subjects had swallowing disorders and 21% subjects were malnourished [18] due to dementia [20] and sarcopenic dysphagia [21].
In this study, elderly patients showed higher flaking skin and atrophy of tongue papillae. Nutritional deficiencies manifest in cells with high turnover rates, such as keratinocytes [22] and may result in skin dryness aspect [23]. Skin desquamation is more common in older patients, ranging from 29% to 58% [24]. Atrophy of tongue papillae is not specific for nutritional deficiencies and it is commonly observed in various clinical conditions [25], including alcoholism [26] and malnutrition [27]. More than one-third of 416 hospitalized elderly presented atrophic glossitis, and it was associated with multiple nutritional deficiencies [28], such as low levels of haemoglobin, ascorbic acid, serum iron and cobalamin [29].
We identified elderly individuals presented higher odds of diseases causing inflammatory stress, reflecting greater severity of the clinical condition and therefore more significant potential in protein metabolism changes. Neuroendocrine and cytokines changes increase the metabolic rate and protein catabolism in response to inflammatory stress to meet the demand for tissue repair and gluconeogenesis [30].
This study has some limitations. Itwas conducted in a tertiary hospital, and many patients were referred from secondary hospitals; thus, it is possible that these patients were previously hospitalized. Because it is a retrospective study, we do not have information about lacking data. It is possible that moderate and severe malnutrition may have been underestimated because patients unable to report were not included in the study. In our study, patients with different diagnosis and treatment were included. Undernutrition correlates with cognitive status and concomitant co-morbidities [4], such as the presence of cancer and infection [9].The results do not represent the elderly population, but only hospitalized older peoplewith severe and debilitating diseases. Besides that, SGA protocol is not specific for elderly patients, and most data are given as binary (yes or no), with no information about the severity. Several studies applied Mini Nutritional Assessment (MNA) in hospitalized elderly, showing a prevalence of nutritional risk around 70% [4-5], higher than other instruments. On the other hand, the large sample size is the strength of our study.
Malnutrition and nutritional risk are common conditions among newly admitted patients in a tertiary hospital, and they are more prevalent in elderly patients. In addition, elderly patients had higher chance of clinical signs of nutritional disorders, anorexia, dysphagia and ingestion of lower energy density foods. These symptoms suggest the oral feeding may be impaired during hospitalization and may aggravate the pre-existing condition. This study suggests a specific approach planning in the integrated geriatric assistance in order to offer early nutritional intervention strategies during hospitalization.
Acknowledgements
We thank (in alphabetical order) Ana Luiza Knudsen Cardoso, Isabela Theófilo Gava, Jana Paula da Silva, Juliana Eiko Yueno, Larissa Godoy, Maísa Bendlin Rockenbach, Mirela Cristina De Marco, Patrícia Cesarino Fram and Stella Maria Franzoni Godoy for their participation in data collection. This research had no funding.
References
- World Health Organization (2015) Summary: World Report on Ageing and Health. Geneva, Switzerland.
- Bozzetti F, Arends J, Lundholm K, Micklewright A, Zurcher G, et al. (2009) ESPEN Guidelines on Parenteral Nutrition: non-surgical oncology. Clin Nutr 28: 445-454.
- Holst M, Yifter-Lindgren E, Surowiak M, Nielsen K, Mowe M, et al. (2013) Nutritional screening and risk factors in elderly hospitalized patients: association to clinical outcome? Scand J Caring Sci 27: 953-961.
- Peng, L, Cheng Y, Chen L, Tung H, Chu K, et al. (2015) Cognition and social physiological factors associated with malnutrition in hospitalized older adults in Taiwan. J Nurs Res 23: 1-5.
- Baek M, Heo Y (2015) Evaluation of the efficacy of nutritional screening tools to predict malnutrition in the elderly at a geriatric care hospital. Nutr Res Pract 9: 637-643.
- Rahman A, Wu T, Bricknell R, Muqtadir Z, Armstrong D (2015) Malnutrition matters in Canadian hospitalized patients: malnutrition risk in hospitalized patients in a tertiary care center using the Malnutrition Universal Screening Tool. Nutr Clin Pract 30: 709-713.
- Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, et al. (1987) What is subjective global assessment of nutritional status? JPENJ Parenter Enteral Nutr 11: 8-13.
- Cunha SFC, Tanaka LS, Salomo RG, Macedo DM, Santos TD, et al. (2015) Nutritional screening in a university hospital: comparison between oncologic and non-Oncologic patients. Food and Nutrition Sciences 6: 75-82.
- Waitzberg DL, Caiaffa WT, Correia MI (2001) Hospital malnutrition: the Brazilian national survey (IBRANUTRI): a study of 4000 patients. Nutrition 17: 573-580.
- Hosmer DW, Lemeshow S (2000) Assessing the Fit of the Model, in Applied Logistic Regression, Second Edition, John Wiley & Sons, Inc., Hoboken, NJ, USA.
- Hughes VA, Roubenoff R, Wood M, Frontera WR, Evans WJ, et al. (2004) Anthropometric assessment of 10-y changes in body composition in the elderly. Am J Clin Nutr 80: 475-482.
- Schneider SM, Al-Jaouni R, Pivot X, Braulio VB, Rampal P, et al. (2002) Lack of adaptation to severe malnutrition in elderly patients. Clin Nutr 21: 499-504.
- Landi F, Lattanzio F, Dell'Aquila G, Eusebi P, Gasperini B, et al. (2013) Prevalence and potentially reversible factors associated with anorexia among older nursing home residents: results from the ULISSE Project. J Am Med Dir Assoc 14: 119-124.
- Soenen S, Chapman IM (2013) Body weight, anorexia, and under nutrition in older people. J Am Med Dir Assoc 14: 642- 648.
- Malafarina V, Uriz-Otano F, Gil-Guerrero L, Iniesta R (2013) The anorexia of ageing: physiopathology, prevalence, associated comorbidity and mortality. A systematic review. Maturita 74: 293-302.
- Sarabia-Cobo CM, Prez V, de Lorena P, Domnguez E, Hermosilla C, et al. (2016) The incidence and prognostic implications of dysphagia in elderly patients institutionalized: a multicenter study in Spain. Appl Nurs Res 30: e6-9.
- Aslam M, Vaezi MF (2013) Dysphagia in the elderly. Gastroenterol Hepatol (NY) 9: 784-795.
- Carrin S, Cabr M, Monteis R, Roca M, Palomera E, et al. (2015) Oropharyngeal dysphagia is a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin Nutr 34: 436-442.
- Hirose T, Hasegawa J, Izawa S, Enoki H, Suzuki Y, et al. (2014) Accumulation of geriatric conditions is associated with poor nutritional status in dependent older people living in the community and in nursing homes. Geriatr Gerontol Int 14: 198-205.
- Rosler A, Pfeil S, Lessmann H, Hder J, Befahr A et al. (2015) Dysphagia in dementia: influence of dementia severity and food texture on the prevalence of aspiration and latency to swallow in hospitalized geriatric patients. J Am Med Dir Assoc 16: 697-701.
- Maeda K, Akagi J (2015) Decreased tongue pressure is associated with sarcopenia and sarcopenic dysphagia in the elderly. Dysphagia 30: 80-87.
- Cunha SF, Gonalves GA, Marchini JS, Roselino AM (2012) Acrodermatitisdueto zinc deficiency after combined vertical gastroplasty with jejunoileal bypass: case report. Sao Paulo Med J 130: 330-335.
- White-Chu EF, Reddy M (2011) Dry skin in the elderly: complexities of a common problem. Clin Dermatol 29: 37-42.
- Smith DR, Sheu HM, Hsieh FS, Lee YL, Chang SJ, et al. (2002) Prevalence of skin disease among nursing home patients in southern Taiwan. Int J Dermatol 41: 754-759.
- Islam NM, Bhattacharyya I, Cohen DM (2011) Common oral manifestations of systemic disease. Otolaryngol Clin North Am 44: 161-182.
- CunhaSF, Melo DA, Braga CB, Vannucchi H, Cunha DF (2012) Papillary atrophy of the tongue and nutritional status of hospitalized alcoholics. An Bras Dermatol 87: 84-89.
- Sheetal A, Hiremath VK, Patil AG, Sajjansetty S, Kumar SR (2013) Malnutrition and its oral outcome-a review. J Clin Diagn Res 7: 178- 180.
- Ehizele AO, Ojehanon PI, Akhionbare O (2009) Nutrition and oral health. Benin Journal of Postgraduate Medicine 11: 76-82.
- Bohmer T, Mowe M (2000) The association between atrophic glossitis and protein- calorie malnutrition in old age. Age Ageing 29: 47-50.
- Bistrian BR (1999) Acute phase proteins and the systemic inflammatory response. Crit Care Med 27: 452-453.