Research Article
Authors:
Saima Ben Fadhel1 and Ana Cristina Diniz Silva2*
1Medical Doctor, University of Sousse, College of Medicine, Sousse, Tunisia
2Department of Postgraduate studies, Dermatology, University of South Wales, UK
Corresponding author
Ana Cristina Diniz Silva, Department of Postgraduate studies, Dermatology, University of South Wales, UK, Tel: +55(31)995864488; E-mail: anacristinadin5@icloud.com; anacristinadinizsilva@gmail.com
Received Date: 28th May 2018; Accepted Date: 14th July 2018; Published Date: 21st July 2018
Citation
Fadhel SB and Silva ACD (2018) Lupus Erythematosus, Dermatomyositis and Systemic Sclerosis: Assessment and Differentials from A Dermatologic Point of View. Enliven: ClinDermatol 4(1): 002
Copyright
@ 2018 Dr. Ana Cristina Diniz Silva. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited
Abstract
Connective tissue diseases (CTDs) are a group of chronic autoimmune conditions characterized by variable involvement of connective tissues, including the skin. Cutaneous manifestations are often observed in the course of lupus erythematosus, dermatomyositis and systemic sclerosis, most commonly as the presenting symptoms. In this paper, we review specific and non-specific symptoms and signs associated with skin involvement in these important CTDs, correlating them with systemic manifestations and laboratory findings, aiming to improve diagnosis accuracy. In the light of evidence-based practice, recommendations for individual assessment and relevant nuances to the differential diagnosis are critically appraised in order to improve diagnosis accuracy and consequently the treatment success.
Keywords
Lupus erythematosus; Dermatomyositis; Systemic sclerosis; Connective tissue diseases; Dermatology
Abbreviations
ACLE: Acute Cutaneous Lupus Erythematosus; ACR: American College of Rheumatology; ANA: Antinuclear Antibodies; Anti-dsDNA: Anti- double-stranded DNA; Anti-La/SSB: Anti-Sjögren's-Syndrome-related antigen B; Anti-RNP: Anti-Ribonucleoprotein; Anti-Ro/SSA: Anti-Sjögren's-Syndrome-related antigen A; Anti-Sm: Anti-Smith; CCLE: Chronic Cutaneous Lupus Erythematosus; CLE: Cutaneous Lupus Erythematosus; CRP: C-Reactive Protein (CRP); CTD: Connective Tissue Disease; DLE: Discoid Lupus Erythematosus; DM: Dermatomyositis; EMG: Electromyography; ENA: Extractable Nuclear Antibody; ESR: Erythrocyte Sedimentation Rate; EULAR: European League Against Rheumatism; ICLE: Intermittent Cutaneous Lupus Erythematosus; IIMs: Idiopathic Inflammatory Myopathies; MCP: Metacarpophalangeal; MCTD: Mixed Connective Tissue Disease; MRI: Magnetic Resonance Imaging; LE: Lupus Erythematosus; RP: Raynaud’s Phenomenon; SCLE: Subacute Cutaneous Lupus Erythematosus; SLE: Systemic Lupus Erythematosus; SSc: Systemic Sclerosis; TEN-like ACLE: Toxic Epidermal Necrolysis-like Acute Cutaneous Lupus Erythematosus.
Introduction
Connective tissue diseases (CTDs) are a group of chronic multiorgan diseases characterized by variable involvement of structural components of connective tissues that have an underlying autoimmune pathogenesis. Lupus erythematosus, dermatomyositis and systemic sclerosis will be the focus of this review, as they constitute the most significant and common CTDs with cutaneous manifestations [1]. Skin signs often represent the preliminary stages of disease and the presenting clinical symptoms. The initial evaluation of CTDs requires a careful history and physical examination, along with selected laboratory testing to identify features that are characteristic of a particular disorder. Additional studies such as diagnostic imaging or biopsy may be necessary. Such testing is dictated by the clinical presentation and differential diagnostic possibilities.
In addition to some specific or even pathognomonic clinical and laboratorial findings, there is also a “nebulous area” around CTDs, consisting of overlapping cutaneous manifestations and auto-antibodies that may confound or hinder the correct diagnosis flow. We consider the present approach crucial in the fields of both dermatology and rheumatology because of the important clinical dilemmas and challenges brought by these conditions to the practitioner, and the impact of such an accurate diagnosis on an individualized and adequate management plan.
The aim of this article is to review the available literature and correlate common and specific cutaneous signs of lupus erythematosus, dermatomyositis and systemic sclerosis to possible systemic manifestations and laboratorial findings. In the light of evidence-based practice, recommendations for individual assessment and relevant nuances to the differential diagnosis are critically appraised in order to improve diagnosis accuracy and consequently the treatment success.
A systematic literature review of the published data between 1979 and 2017 was conducted using the key words “dermatology” or “cutaneous manifestations” and “lupus erythematosus” or “dermatomyositis” or “systemic sclerosis” or “connective tissue diseases”. In this paper, we analyzed 33 references, including the most relevant systematic reviews, case reports, prospective cohorts and retrospective studies, related to our main objective, i.e., provide the clinician with an objective and practical guidance to an accurate diagnosis of the most common CTDs from a dermatologic point of view.
Discussion
Clinical Presentation
Lupus Erythematosus
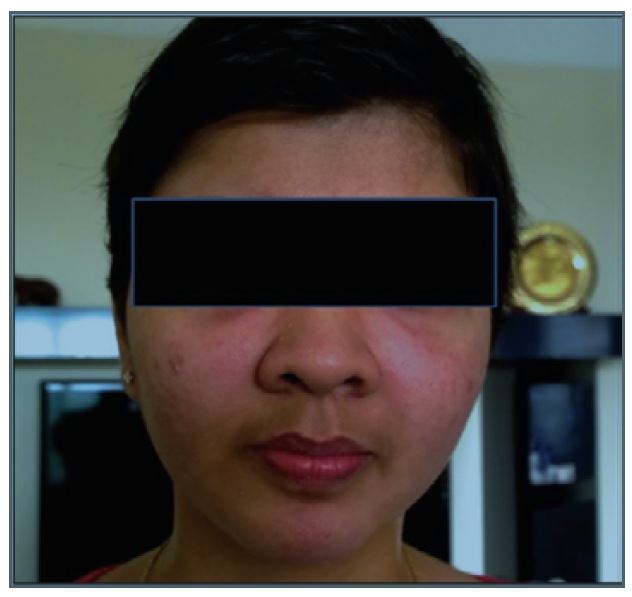
Lupus erythematosus (LE) is an autoimmune disease of unknown etiology that can have many clinical manifestations. LE can be divided into a systemic and a cutaneous form (SLE and CLE) [2]. The skin is the second most commonly affected organ, following joints. It is involved in up to 75% of patients with SLE, and may be the first sign of disease in 25% of patients [2]. In the 1997 American College of Rheumatology classification criteria for SLE, four out of 11 diagnostic criteria are muco-cutaneous manifestations, including malar and discoid rashes, photosensitivity, and nasal/oral ulcerations) [3]. Malar rash (diagnosis sensitivity 57%; specificity 96%) is a butterfly-shaped erythematous rash that can be flat or rose over the cheeks and bridge of the nose (Figure 1) [4]. It lasts from days to weeks and is occasionally painful or pruritic [3]. Photosensitivity (diagnosis sensitivity 43%; specificity 96%) is characterized by the development of a macular or a diffuse erythematous rash in sun-exposed areas as a result of the exposure to ultraviolet light that usually persists for more than one day. It can also present as erythematous papules or macules on the dorsal aspects of the hands, classically sparing the knuckles [3]. Discoid rash (diagnosis sensitivity 18%; specificity 59%) is characterized by disc-shaped, erythematous plaques of varying size, containing areas of follicular hyperkeratosis, which are painful if lifted manually [3]. Oral ulcers tend to occur in crops. They are usually shallow, with 1-2cm in diameter [3].
Figure 1:Malar rash: a butterfly-shaped erythematous rash over the cheeks and bridge of the nose [4].
The classification of CLE can be difficult and confusing. However, in 1979, the American dermatologists Gilliam and Sontheimer proposed an improved classification that has become widely accepted [5]. Based on histopathological findings, the cutaneous manifestations of LE can be divided into LE-specific and LE-non-specific skin manifestations. While the LE-specific skin manifestations show a typical histopathological picture with a lichenoid tissue reaction, LE-non-specific presentation includes a wide range of symptoms with different histopathological pictures, which are not exclusive to lupus disease since they can be seen in several other autoimmune diseases [6]. Lupus-specific skin lesions serve primarily as an important diagnostic clue, whereas lupus non-specific skin lesions are associated with more active disease [6].
LE-specific skin manifestations encompass 4 different subtypes: acute CLE, subacute CLE, chronic CLE and a recently defined entity, intermittent CLE, which now includes lupus erythematosus tumidus [2,3,7]. These subtypes are primarily distinguished by morphological and histological findings, as shown in Table 1 [2,3,7-9]. LE non-specific skin manifestations are summarized in Table 2 [2,3,7].
|
Subtypes |
Characteristics |
|
*Localized: ‘’butterfly rash’’ |
|
*Annular and/or papulosquamous/psoriasiform with polycyclic confluence |
|
|
|
*Discoid erythematous plaques with firmly adherent follicular hyperkeratosis |
|
*Only 2% of CLE patients present with this form |
|
*subcutaneous, nodular/plaque-like, dense infiltrates |
|
*Oral DLE: lesions occur most commonly on the labial mucosa, vermillion border and buccal mucosa, characterized by white papules, central erythema, irradiating white striae and peripheral telengiectasia. |
|
*tender, livid red swelling, sometimes with erosion/ulceration |
|
Lupus Erythematosus/Lichen Planusoverlap syndrome (lupus planus) |
|
|
|
Lupus tumidus |
*Erythematous, urticaria-like edematous plaques without epidermal involvement |
Table 1: Lupus erythematosus specific skin manifestation, based on the modified Gilliam and Dusseldorf Classification for Cutaneous Lupus [2,3,7-9]
|
Skin manifestations |
Characteristics |
|
*Lupus hair/Telogen effluvium/Alopecia areata |
|
|
|
Sclerodactyly, rheumatoid nodules, calcinosis cutis, urticaria, acanthosis nigricans, erythema multiforme, leg ulcers, papulonodular mucinosis and cutis laxa, LE-nonspecific bullous lesions |
Table 2: Lupus erythematosus non-specific skin manifestation, based on the modified Gilliam and Dusseldorf Classification for Cutaneous Lupus [2,3,7]
Dermatomyositis
Dermatomyositis (DM), a subtype of Idiopathic Inflammatory Myopathies (IIMs), is a disorder that includes characteristic skin rash, proximal muscle weakness and inflammatory infiltrates in the muscle tissue [10]. The skin manifestations of DM are the most important aspect of the disease. Their correct evaluation is important for early diagnosis, and to measure disease activity [10]. A proportion of patients will have the characteristic cutaneous findings of DM, and never develop clinical or laboratory signs of myositis [11]. According to Reeder, et al., [11] these clinically amyopathic dermatomyositis represents about 20% of all dermatomyositis cases. DM skin manifestations are generally grouped as pathognomonic, characteristic, compatible, less common and rare [12].
The pathognomonic cutaneous manifestations of DM are Gottron’s papules and Gottron’s sign. Gottron's papules consist of erythematous to violaceous papules and plaques over the extensor surfaces of the metacarpophalangeal and interphalangeal joints (Figure 2) [12,13]. These lesions may have accompanying scale, and can sometimes develop ulcerations. Active lesions tend to resolve with dyspigmentation, atrophy, and scarring [12]. Gottron’s papules occur in approximately 70% of patients with DM. Gottron’s sign refers to symmetric, usually non-scaling, violaceous erythematous macules and patches over the extensor surfaces of the elbows and/or knees. Theses lesions are often atrophic [14].
Figure 2:Gottron’s papules: erythematous to violaceous papules and plaques over the extensor surfaces of the metacarpophalangeal and interphalangeal joints, a pathognomonic sign of dematomyositis [13].
Highly characteristic lesions include violaceous erythema of the upper eyelids, the heliotrope rash, which is often accompanied with edema and telangiectasiae (Figure 3) [14,15]. Other typical findings include an erythematous macular rash on the face, neck, and chest, called the “V sign” or on the back of the neck and shoulders (shawl sign), ragged cuticles and periungual telangiectasias [14]. Characteristic hand lesions include rough and cracked, hyperkeratotic, "dirty" horizontal lines on the lateral and palmar areas of the fingers, resembling "mechanics" hands. These lesions are photosensitive and commonly pruritic [16]. Non-sun-exposed areas can also be involved, especially the scalp, lower back, and lateral thighs (Holster sign) [10].
Figure 3:Heliotrope rash: violaceous erythema of the upper eyelids, highly characteristic of dermatomyositis [15].
Poikiloderma atrophicansvasculare is a manifestation of disease chronicity with a mottled pattern of hyper pigmented and hypo pigmented macules interspersed with telangiectasiae [14]. Calcinosis cutis (calcium deposition) occurs in 30 to 70% of cases of juvenile DM and in only 10% of adult cases [17]. Calcinosis is most commonly present on the buttocks, elbows, knees or traumatized areas, and is associated with increased disease activity and duration [14].
Less common manifestations include facial swelling, malignancy, erythroderma, lichen planus, cutaneous vasculitis and panniculitis [12]. Rare manifestations include follicular hyperkeratosis, papular mucinosis, hypertrichosis, malignant erythema, urticaria/urticarial vasculitis, partial lipodystrophy, malignant atrophic papulosis (Degos' disease), zebra-like striping and vulvar/scrotal skin changes [12].
Systemic Sclerosis
Systemic sclerosis (SSc) is multisystem disorder characterized by abnormalities of vasculature, immune system, and extracellular matrix that lead to fibrosis of the skin and internal organs. Systemic involvement may occur in the form of pulmonary vasculopathy, interstitial fibrosis, myocardiopathy, arrhythmia, conduction abnormality, acute renal crisis, lower esophageal incompetence, among others [18].
The skin is almost always involved in SSc. In localized form of SSc (sometimes referred to as the CREST syndrome meaning calcinosis, Raynaud’s phenomenon, esophageal involvement, sclerodactyly and telangiectasia), skin changes affect predominantly the face and hands (Figure 4) [19,20]. Diffuse SSc, which is less common than the localized form, denotes more widespread skin involvement proximal to the elbows and knees [21].
Figure 4:Sclerodactily characterized by thickening and tightening of the skin of the digits [20].
One of the first signs of the disease is Raynaud's phenomenon (RP), which occurs in almost all cases (95%) [22]. RP manifests as episodic pallor followed by cyanosis and/or rubor of the distal portions of the digits after exposure to cold or emotional stress. It usually predates other manifestations in the limited subtype and is often found concurrently in diffuse SSc [22].
The skin develops a diffuse, hard texture, which is difficult to pinch (hide bound skin) and its surface becomes smooth, taut, causing the “mask-like facies”. Similarly, the nasal alae become atrophied, resulting in a pinched appearance to the nose, the so-called “mouse facies”. The oral manifestations include microstomia, xerostomia, telangiectasia, and perioral furrowing (“purse-string”mouth) [23]. The inability to retract the lower eye-lid due to underlying sclerosis (Ingram's sign) may coexist [24]. Skin over the extremities, faces, and trunk may become darkly pigmented and contrasting areas of hypo pigmentation may also develop. The sparing of pigment around hair follicle gives the skin a “salt and pepper” appearance [23]. Other findings include nail-fold capillary abnormalities, characterized by telangiectasia, dilated loops at the nail bed and distended venules [25].
The abnormal deposition of calcium in soft tissues independent of the plasma levels of calcium and phosphorous (calcinosis) is a frequent finding in SSc [22]. Dystrophic calcification of acral distribution (digits, elbows, knees) is the most common type of calcinosis associated to SSc. It occurs in approximately 25% of patients causing pain, local inflammation, irritation, muscle atrophy, ulceration with the possibility of secondary infection, and joint contractures [22].
Involvement of the hands in SSc includes digital pitting scars with resorption of the terminal phalanges (acro-osteolysis), and flexion contractures that produce shortened claw-like fingers [26]. Ulceration of the finger tips due to abnormal collagen deposition is the hallmark of SSc-related vasculopathy and is characterized by endothelial dysfunction leading to intimal proliferation and thrombosis [27]. Digital ulcers are painful, heal slowly and are a major clinical problem in patients with limited or diffuse SSc, occurring in 30 and 58% patients, respectively. Digital ulcers are considered a marker for disease severity [22].
Differential Diagnosis
Lupus Erythematosus
As part of the medical history and physical examination, we should pay particular attention to specific symptoms and signs, which are shown in Table 3. Laboratory investigations that support the diagnosis of LE are summarized in the same table [28-30].
|
History |
A history of exposure to medications associated with drug-induced lupus such as hydralazine, minocycline, procainamide and anti-tumor necrosis factor (TNF) agent. |
|
Physical examination |
*Photosensitive skin lesions such as a malar rash or discoid lesions |
|
Laboratory investigations |
*If SLE is suspected clinically, antinuclear antibodies (ANA) are performed |
Table 3: Medical history, symptoms and laboratory tests suggestive of lupus erythematosus [28-30]
Dermatomyositis
The investigations begin with a careful history and physical examination, as well as selected laboratory testing. Key points in the history include the onset, duration and characteristics of the muscle weakness as well as the accompanying symptoms: a history of dysphagia may suggest esophageal involvement and a history of cough or shortness of breath is suggestive of pulmonary involvement [31].
Physical examination aims to identify characteristic cutaneous manifestations. It should also include heart and lung auscultation for evidence of interstitial disease, and neurologic and neuromuscular examination to determine the severity and distribution of weakness and/or muscle tenderness, as well as the presence or absence of other abnormal neurologic findings [31]. Joint examination may reveal signs of inflammatory arthritis. Chest X-Rays should be performed in all patients with findings suggesting DM to help in detecting the presence of pulmonary involvement [31].
General laboratory testing usually includes a complete blood count with differential, creatinine, ESR, CRP, liver function tests, and thyroid-stimulating hormone (TSH) [31]. In addition, testing for muscle enzymes (creatine kinase and aldolase) should be performed as well as specific ANA (anti-Ro/SSA, anti-La/SSB, anti-RNP, and anti-Sm), and myositis-associated antibodies, including anti-Jo-1 and other anti-synthetase antibodies [31].
Generally, these characteristic clinical and laboratory findings are sufficient for the diagnosis of DM. However, additional data, such as magnetic resonance (MRI), electromyography (EMG), skin biopsy and muscle biopsy, may be necessary to confirm the diagnosis, especially in those patients who present with typical muscle weakness, in the absence of specific cutaneous manifestations or myositis-specific antibodies (MSA) [31].
Systemic Sclerosis
The mainstay for the diagnosis of SSc remains the clinical presentation. The ACR/EULAR has proposed criteria to assist in identifying those affected with the condition, as shown in Table 4 [32].
|
Item |
Sub-items |
Score |
|
Skin thickening of the fingers of both hands extending proximal to the metacarpal (MCP) joints (sufficient criterion) |
- |
9 |
|
Fingertip lesions (only count the higher score) |
*Puffy fingers |
2 |
|
Fingertip lesions (only count the higher score) |
*Digital tip ulcers |
2 |
|
Telangiectasia |
- |
2 |
|
Abnormal nailfold capillaries |
- |
2 |
|
Pulmonary arterial hypertension and/or interstitial lung disease (maximum score is 2) |
*Pulmonary arterial hypertension |
2 |
|
Raynaud’s phenomenon |
- |
3 |
|
Ssc related autoantibodies (maximum score is 3) |
*Anticentromere 3: positive in about 60% of limited cutaneous disease, specific, but not sensitive |
3 |
|
The total score is determined by adding the maximum weight in each category. |
||
Table 4: 2013 ACR/EULAR criteria for the diagnosis of systemic sclerosis [32]
Several investigations can provide additional information for classification and prognostication. These include blood tests (complete blood count, blood glucose and inflammatory markers) and the evaluation of specific target organs: lung fibrosis and restrictive lung disease (chest X-Rays, spirometry studies and lung biopsy), joints (X-rays), liver (serum albumin), kidneys (blood urea, creatinine, and electrolytes) and heart (echocardiography) [33].
Conclusion
Lupus erythematosus, dermatomyositis and systemic sclerosis are inflammatory autoimmune diseases which may affect several organs simultaneously, including the skin. In SLE, the skin is the second most commonly affected organ, following the joints. In fact, four out of the 11 SLE diagnostic criteria consist of muco-cutaneous manifestations, including malar and discoid rashes, photosensitivity, and nasal/oral ulcerations. Gottron’s papules and Gottron’s sign are pathognomonic manifestations of DM, whereas heliotrope rash is known as a typical aspect of this condition. The correct identifications of these signs are pivotal for both early diagnosis and as a measure of disease activity.
The skin is almost always involved in systemic sclerosis. In the localized form, Raynaud's phenomenon, sclerodactyly and telangiectasia are often observed, affecting predominantly the hands. Diffuse SSc, in contrast, widespread skin involvement occurs proximally to the elbows and knees. It is characterized by a taut, smooth skin surface that becomes difficult to pinch.
In conclusion, given that these CTDs commonly exhibit significant skin manifestations several months to years before the systemic manifestations, the dermatologist has a crucial role to play. A good knowledge of such clinical signs could, indeed, guide further biological and immunological studies, thus contributing to an earlier diagnosis and proper management plan.
References
- Reddy BY, Hantash BM (2009) Cutaneous Connective Tissue Diseases: Epidemiology, Diagnosis, and Treatment. Open Dermatol J 3: 22-31.
- Hersh AO, Arkin LM, Prahalad S (2016) Immunogenetics of Cutaneous Lupus Erythematosus. Curr Opin Pediatr 28: 470-475.
- Uva L, Miguel D, Pinheiro C, Freitas JP, Marques Gomes M, et al. (2012) Cutaneous Manifestations of Systemic Lupus Erythematosus. Autoimmune Dis 2012: 834291.
- Chandra SR, Issac TG, Ayyappan K (2015) New onset psychosis as the first manifestation of neuro-psychiatric lupus. A situation causing diagnostic dilemma. Indian J Psychol Med 37: 333-338.
- Sontheimer RD, Thomas JR, Gilliam JN (1979) Subacute cutaneous lupus erythematosus: A cutaneous marker for a distinct lupus erythematosus subset. Arch Dermatol 115:1409-1415.
- Grönhagen CM, Nyberg F (2014) Cutaneous lupus erythematosus: An update. Indian Dermatol Online J 5: 7-13.
- Kuhn A, Bonsmann G, Anders H-J, Herzer P, Tenbrock K, et al. (2015) The Diagnosis and Treatment of Systemic Lupus Erythematosus. Dtsch Ärztebl Int 112: 423-432.
- Ranginwala AM, Chalishazar MM, Panja P, Buddhdev KP, Kale HM (2012) Oral discoid lupus erythematosus: A study of twenty-one cases. J Oral Maxillofac Pathol 16: 368-373.
- Romiti R, Anzai A, Nico MM (2014) Genital discoid lupus: a rare manifestation of cutaneous lupus erythematosus. Lupus 23: 707-710.
- Stephens D, Schwarzenberger K, Jones C, Cooper S (2015) The Holster Sign: An Overlooked Cutaneous Finding in the Diagnosis of Dermatomyositis. J Arthritis 4: 145.
- Bendewald MJ, Wetter DA, Li X, Davis MD (2010) Incidence of Dermatomyositis and Clinically Amyopathic Dermatomyositis: A Population-Based Study in Olmsted County, Minnesota. Arch Dermatol 146: 26-30.
- Koler RA, Montemarano A (2001) Dermatomyositis. Am Fam Physician 64: 1565-1572.
- Lamquami S, Errarhay S, Mamouni N, Bouchikhi C, Banani A (2015) Dermatomyositis revealing breast cancer: report of a case. Pan Afr Med J. 21: 89.
- Marvi U, Chung L, Fiorentino DF (2012) Clinical Presentation and Evaluation of Dermatomyositis. Indian J Dermatol 57: 375-381.
- Dias LP, Faria AL, Scandiuzzi MM, Inhaia CL, Shida JY, et al., (2015) A rare case of severe myositis as paraneoplastic syndrome on breast cancer. World J Surg Oncol. 13: 134.
- Khan S, Christopher-Stine L (2011) Polymyositis, dermatomyositis, and autoimmune necrotizing myopathy: clinical features. Rheum Dis Clin North Am 37: 143-158.
- Maan MA, Akhtar SJ, Haque H (2008) Dermatomyositis. Journal of Pakistan Association of Dermatologists 18: 33-43.
- Singh A, Ambujam S, Varghese A, Vishranth SP, Sadanandan N (2012) Salt-and-pepper Appearance: A Cutaneous Clue for the Diagnosis of Systemic Sclerosis. Indian J Dermatol 57: 412-413.
- Graham-Brown R, Harman K, Johnston G (2016) Lecture Notes: Dermatology (11th edition) Wiley-Blackwell, Hoboken, New Jersey, USA.
- Russo RA, Katsicas MM (2007) Clinical characteristics of children with Juvenile Systemic Sclerosis: follow-up of 23 patients in a single tertiary center. Pediatr Rheumatol Online J. 5: 6.
- Alhajeri H, Hudson M, Fritzler M, Pope J, Tatibouet S, et al., (2015) 2013 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Systemic Sclerosis Outperform the 1980 Criteria: Data From the Canadian Scleroderma Research Group. Arthritis Care Res 67: 582–587.
- Vitiello M, Abuchar A, Santana N, Dehesa L, Kerdel FA (2012) An Update on the Treatment of the Cutaneous Manifestations of Systemic Sclerosis: The Dermatologist’s Point of View. J Clin Aesthet Dermatol 5: 33-43.
- Jagadish R, Mehta DS, Jagadish P (2012) Oral and periodontal manifestations associated with systemic sclerosis: A case series and review. J Indian Soc Periodontol, 16: 271–274.
- Madke B, Nayak C (2012) Eponymous signs in dermatology. Indian Dermatol Online J 3: 159-165.
- Rossi A, Sozio F, Sestini P, Renzoni EA, Khan K, et al., (2010) Lymphatic and blood vessels in scleroderma skin, a morphometric analysis. Hum Pathol 41: 366-374.
- Anbiaee N, Tafakhori Z (2011) Early diagnosis of progressive systemic sclerosis (scleroderma) from a panoramic view: report of three cases. Dentomaxillofac Radiol 40: 457-462.
- Schiopu E, Impens AJ, Phillips K (2010) Digital Ischemia in Scleroderma Spectrum of Diseases. Int J Rheumatol 2010: 923743.
- Wallace DJ (2017) Diagnosis and differential diagnosis of systemic lupus erythematosus in adullts.
- Merola JF (2017) Drug-induced lupus. Uptodate.
- Egner W (2000) The use of laboratory tests in the diagnosis of SLE. J Clin Pathol 53: 424-432
- Miller ML (2017) Diagnosis and differential diagnosis of dermatomyositis and polymyositis in adults.
- Adigun R, Bhimji SS (2017) Systemic Sclerosis (CREST syndrome). StatPearls.