Research Article
Kuldar Kaljurand, MD*
Eye Clinic of Tartu University Clinics, Estonia
Corresponding author
Kuldar Kaljurand, Eye Clinic of Tartu University Clinics, J. Kuperjanovi, 1 Tartu Estonia 51003; Tel: +3737319762; Fax: +3727319754; E-mail: Kuldar.Kaljurand@kliinikum.ee
Received Date: 15th December 2014
Accepted Date: 11th February 2015
Published Date: 16th February 2015
Citation
Kaljurand K (2015) Efficacy of the Selective Laser Trabeculoplasty in Exfoliation and Primary Open-Angle Glaucoma. Enliven: Clin Ophthalmol Res 1(1): 002.
Copyright
@2015 Dr. Kuldar Kaljurand. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: This is comparative study for evaluation of the efficacy and lastingness of intraocular pressure (IOP) reduction of selective laser trabeculoplasty (SLT) in exfoliation (EG) and primary open-angle (POAG) glaucoma.
Methods: 48 patients with EG and 48 with POAG were recruited to the study. The angle grade 3 and 4, by Shaffer, were considered to be open. Trabecular meshwork (TM) pigmentation was graded from 0 = no pigmentation, to 4 = dense pigmentation. TM was treated with a 532-nm frequency-doubled, Q-swiched Nd:YAG laser, energy ranged from 0.7 to 2.0 mJ. IOP were measured during one year follow-up.
Results: Patients in the EG group were older than in POAG group and had significantly more pigmented TM. The mean baseline IOP in the EG group was 24.1 (± 4.5) and 23.7 (± 3.3) in the POAG group and in the end of the one-year follow-up 18.6 (± 3.7) and 18.4 (± 2.5) mmHg respectively with no significant difference between two groups. The 12-month success rate was 87.3% and 69.7% in the EG and POAG patients, p= 0.05. Interaction between exfoliation syndrome (EXS) and the energy of the laser, not the level of TM pigmentation was significant predictor of the IOP rise during the follow-up. The odds of a relapse are 2.98 times lower for patients with EXS.
Conclusions: SLT is effective and reduction of IOP is long-lasting in EG and POAG patients. Exfoliative material independently from TM pigmentation seems to have influence to results of SLT.
Keywords
Exfoliaton syndrome; Glaucoma; Selective laser trabeculoplasty; Intraocular pressure
Introduction
Since it was standardised by Wise and Winter laser trabeculoplasty has been a good working tool in the hands of glaucoma specialists. Selective laser trabeculoplasty (SLT) uses a 532-nm Q-switched frequency-doubled Nd:YAG laser with single pulse of short duration and low fluency [1]. SLT is a procedure that selectively targets pigmented trabecular meshwork (TM) cells without causing thermal or collateral damage to non-pigmented cells and structures [1]. Although the exact mechanism of SLT is not completely understood it appears to be a safe and effective method to lower IOP in eyes with open-angle glaucoma [2-5]. The present prospective clinical trial compared the IOP response and lastingness of the effect to SLT of exfoliation glaucoma (EG) and primary open angle glaucoma (POAG).
Patients and Methods
Patients were recruited from the out-patient department of the Eye Clinic of Tartu University Clinics. The study comprised EG and POAG patients in medical treatment with uncontrolled or additional need for lower intraocular pressure (IOP) to reach the target pressure. Both groups included 48 eyes of 48 patients. All patients underwent baseline examinations including biomicroscopy, fundusscopy, computerised perimetry and Goldmann?s applanation tonometry. Gonioscopies were performed on all patients and angle grade 3 and 4, by Shaffer, were considered to be open and were included in the study. Trabecular meshwork pigmentation was graded according to a standard scale that ranged from 0 = no pigmentation, to 4 = dense pigmentation. Past and present ocular medication and ocular history was recorded, as were age and gender. Patients with any kind of previous ocular surgery, trauma and uveitis or chronic inflammation conditions were not included. None of the patients had undergone a previous laser trabeculoplasty procedure.
The trabecular meshwork of each eye was treated with a 532-nm frequency-doubled, Q-swiched Nd:YAG laser (ARC Q-LAS 10) by one surgeon (KK). Latina single-mirror goniolens were used to perform laser applications. The single-pulse duration was 3 ns and the spot size was 400 ?m in all cases. Treatment was conducted with adjacent but not overlapping spots. The initial energy was set at 0.7 mJ and was raised until cavitation bubbles formed and treated at this energy level. The pulse energies ranged from 0.7 to 2.0 mJ.
IOP were measured and one drop of Pilocarpine 2% was instilled in the eye 25?30 minutes before treatment. No anti-inflammatory agents were prescribed after treatment. All patients underwent a slit-lamp examination and applanation tonometry one hour after surgery in order to assess the anterior chamber reaction and IOP spikes. IOP were measured one day, one week, one month, three and six months and one year after the procedure. The windows for follow-up visits were ± 1 day for the one- week visit, one week for the one-, three-, and six-month visits and one month for the one-year visit. At each visit, patients were invited to report any symptoms of ocular morbidity and ophthalmic examination was performed including visual acuity, biomicroscopy, applanation tonometry and gonioscopy. Visual field assessment by computerized perimetry was performed 1-3 weeks before the procedure, six and 12 months after the SLT procedure and in cases with insufficient IOP reduction before additional medical treatment or filtering surgery.
Treatment was considered to be effective when a 20% decrease was obtained in the IOP after the one-year follow-up period compared to the baseline values with no additional anti-glaucomatous interventions. Failure was defined as an IOP reduction of less than 20% from baseline at the follow-up. Any change in hypotensive medication or need for filtering surgery during a follow-up led to the patients? is being excluded from further analysis. The study was performed in accordance with the ethical standards laid down in the Declaration of Helsinki and approved by local Ethic Committee.
Results
In both groups, 11 patients flailed to respond to SLT (non-responders, decrease of IOP < 20% after follow-up; Table 1). There was no difference between genders in both groups among the non-responders. Patients in the EG group were significantly older than those in POAG-group. Both groups had the same male/female ratio and a similar number of preoperative hypotensive medications. The mean baseline IOP in the EG group was 24.1 (± 4.5) and 23.7 (± 3.3) in the POAG group.
| EG | POAG | P | |
| Patients/eyes recruited (No.) | 48 | 48 | = 1.0? |
| Non-responders (No.) | 11 | 11 | = 0.8?* |
| Age (years) [SD] | 74.3 [9.2] | 70.4 [5.4] | = 0.04? |
| Gender: | |||
| Male | 8 | 10 | |
| Female | 29 | 26 | |
| Baseline IOP | 24.1 [± 4.5] | 23.7 [± 3.3] | = 0.06? |
| TM pigmentation (mean) [SD] | 2.4 [0.6] | 1.8 [0.8] | = 0.04? |
| Hypotensive medication (mean) [SD] | 2.2 [0.8] | 2.1 [0.8] | = 0.89? |
Table 1: Baseline Characteristics
EG: Exfoliative glaucoma; POAG: Primary open-angle glaucoma; [SD]: Standard deviation; IOP: intraocular pressure; TM: trabecular meshwork; p: ? t-test; ? Fisher?s exact test *One patient from the POAG group underwent cataract surgery during the follow-up time and was excluded.
The difference between trabecular meshwork (TM) pigmentation was statistically significant; patients with EXS had more pigmented anterior chamber angles, p= 0.04 (Table I). In the POAG group 15% and 39% of EXS-group patients had TM pigmentation grade >2 by Shaffer. The energy used in the POAG group was higher than in the EG group but not statistically significantly (Table 2).
| EG | POAG | P | |
| Number of applications [SD] | 80.5 [17.2] | 74.2 [18.5] | 0.16 |
| Mean energy of spot, mJ [SD] | 1.42 [0.4] | 1.54 [0.4] | 0.27 |
| Treatment area | 360º | 360º | |
| Spot size (?m) | 400 | 400 | |
| Pulse duration (ns) | 3 | 3 |
Table 2: Intraoperative Parameters
EG: Exfoliative glaucoma; POAG: Primary open-angle glaucoma; SD: Standard deviation; mJ: mill Joule; ?m: micrometer; p: paird t-test
In all eyes of both groups, treatment was conducted on a 360º adjacent and not overlapping spots. Difference of received applications was statistically not significant. Table 2 lists the intraoperative characteristics of both groups. Postoperative IOP rise, measured 1h after procedure, was presented in 43% of patients in the EG group and in 33% of patients in the POAG group, p > 0.05. The IOP elevations over 4 mmHg (8 in EG and 9 in POAG group) were covered by a single dose of per oral Acetozolamide 250 mg. All postoperative IOP elevations were resolved within 24 hours. The responders mean IOP and mean IOP reduction in percentage from baseline at different intervals after treatment are listed in Table 3.
| Mean IOP mmHg [SD] | Mean % IOP Reduction | |||||
| EG | POAG | p | EG | POAG | ||
| Baseline | 24.1 [4.5] | 23.7 [3.3] | > 0.05 | |||
| 1 hour | 25.2 [5.7] | 24.8 [6.4] | > 0.05 | -4.1 | -4.6 | |
| 1 day | 16.4 [2.8] | 17.8 [6.4] | > 0.05 | 31.9 | 24.9 | |
| 1 week | 21.7 [4.9] | 20.8 [4.1] | > 0.05 | 9.9 | 12.3 | |
| 1 month | 17.7 [3.5] | 19.8 [4.9] | 0.05 | 26.6 | 16.5 | |
| 3 months | 18.8 [3.8] | 21.1 [4.2] | 0.03 | 22 | 11 | |
| 6 months | 19.7 [3.1] | 19.0 [3.6] | > 0.05 | 18.2 | 19.8 | |
| 1 year | 18.6 [3.7] | 18.4 [2.5] | 0.7 | 21.5 | 20.2 | |
Table III: Mean IOP and Mean IOP Reductions of Responders from Baseline at Different Intervals after Treatment (in Percentage)
IOP: Intraocular pressure; SD: Standard deviation; EG: Exfoliative glaucoma; POAG: Primary open-angle glaucoma; p: paired t-test
The mean IOP reductions were significantly smaller in the POAG group at first and third months of follow-up. No significant difference was found between two groups for mean IOP at the end of the follow-up.
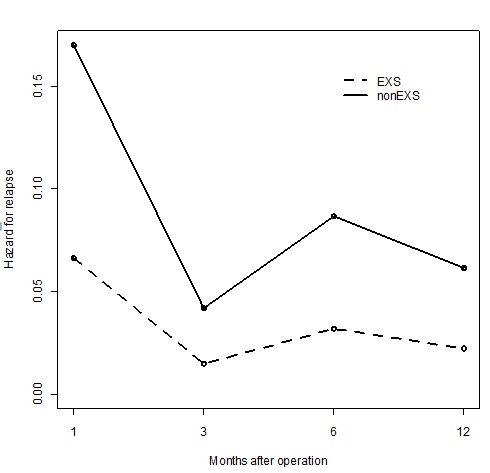
In order to estimate the permanency of the pressure-lowering effect of SLT, discrete time survival analysis was performed using logistic regression models. The survival event was defined as the first occurrence of relapse, where a patient?s post-operative IOP was more than 80% of their pre-operative IOP. There was statistically significant difference (< 0.01) between the two groups in terms of the risk of relapse following the formula: h(t)= 1/(1+exp(-(Mt +0.935 x (power of the laser beam) -1.059 x I(EXS))) where Mt denotes the effect of time period t , and I(EXS) equals 1, if the patient EXS and 0 if has not; (Figure 1).
Figure I: Survival analysis for the EG and the POAG group
On average, the odds of a relapse are 2.98 times lower for patients with EXS than those without it. The 12-month success rate was 87.3% in the EG and 69.7% in the POAG group (95% CI, 2.0-25.1), with a statistically significant difference between the two groups.
A backward selection procedure on full model (including variables as presence of EXS, TM pigmentation, number of applications, energy of the laser beam and age) was performed in order to determine the significant effects of the variables. This resulted in a model in which the interaction between EXS and the energy of the laser (Markov chain Monte-Carlo; 95% CI -0.2--6.7), but not the level of TM pigmentation, were statistically significant predictors of the hazard for IOP rise, (p = 0.04). According to this model, neither the number of applications nor the energy of the laser beam influenced to the SLT success rate in the two groups.
There were no significant complications in the patients of both groups. None of the patients complained of serious discomfort or pain during treatment. There was moderate irritation in the treated eye at one hour after the treatment. Patients reported that they ?felt their eye? a few days postoperatively. After the one-week follow-up there were no signs (0 cells) of inflammation in anterior chamber or conjunctive reaction in both groups. Patients did not receive any anti-inflammatory medication after the procedure. No cases of peripheral anterior synechiaes (PAS) forming were noted in either group during the duration of the study.
Discussion
Laser trabeculoplasty is a widely used and commonly accepted procedure for lowering IOP in eyes with medically uncontrolled open-angle glaucoma. During a last-decade SLT, a 532-nm Q-switched frequency-doubled Nd:-YAG laser has been successfully employed in the treatment of open-angle glaucoma [6,7]. SLT can be used in cases of uncontrolled IOP [8] as a replacement for medical therapy [9] and even as first-line therapy [8,10].
Exfoliation syndrome (EXS) and EG are relatively frequent findings in Northern Europe, Scandinavia and other parts of the world [11-15].
EG as secondary open-angle glaucoma is treated with the same principles as POAG, although it has more aggressive natural course [16,17] Regrettably, EG is harder to control as it responds less efficiently to medical therapy [16]. SLT, as safe and repeatable [5] method, appears to be an effective method of lowering IOP in POAG and EG cases.
There are several theories with which to explain the mechanism of the laser trabeculoplasty. According to evidence, SLT does not cause structural alterations in the TM [1,18,19]. The biologic theory suggests that lowered IOP is the result of the thermal energy the laser stimulating cellular activity [20,21]. This can initiate a chain of events that upregulates expression, which is a trigger for remodeling the extracellular matrix in the TM and a release of chemotactic and vasoactive agents. The study by Cellini et al. focused on the matrix metalloproteinase-2 (MMP-2) and the tissue inhibitors of metalloproteinase-2 (TIMP-2) values in aqueous humor of the anterior chamber and found a significant increase in patients with EXS compared to controls and this imbalance could be a reason for disability to decrease the IOP in EG [22]. In the present study, as in many others [11,13,16] the mean baseline IOP was higher (but not significantly) in EG patients than in POAG patients. According to Dr. Cellini study one explanation for that can be an elevated TIMP-2/MMP-2 ratio in EXS-patients [22]. Contrarily to his findings we found a more stable SLT IOP-lowering effect on EG patients compared to POAG. Inhabitants of Estonia generally have blue or blue-gray irises and relatively light anterior chamber angle pigmentation. In the present study, patients in the EG group had significantly greater degree of TM pigmentation than the POAG group (Table 1). The mean percent of IOP reduction was greater in the (more pigmented) EG group at the first and third postoperative month but the difference stabilized at the end of the follow-up (Table 3). Chen et al. found that the pigmentation at the TM is significantly related to the pressure-lowering effect of SLT at least seven month after treatment [23]. Gra?ner et al. found a negative correlation between lower TM pigmentation and SLT success in POAG patients [24]. Contrarily of the two above mentioned two studies, the present study?s logistic regression analysis did not find a significant influence of TM pigmentation on IOP, which agrees with some other studies [8,25], either separately or in interaction with used energy level and number of applications in both groups. Hodge et al. [25] found that patients in a success group (IOP reduction >20%) and non-success group (IOP reduction < 20%) did not differ in the degree of TM pigmentation. The present study found that presence of EXS, independently form the degree of TM pigmentation, had a significant influence for the continuous pressure-lowering effect of SLT.
According to SLT procedure-protocol the energy of the laser beam is raised until bubble formation occurs on a TM. The laser beam energy-level used in the more pigmented, EG group was lower, although not significantly. Due to the relatively light pigmentation of TM in both groups, a proportionally high energy laser beam was used to achieve a therapeutic effect. Higher energy could be a causative factor for patho-physiological reactions, which can explain the rapid increase of the IOP in the first hour and the decrease 24 hours after the procedure. However, the exact mechanism of SLT is still unclear and further investigations are needed in order to clarify this issue.
In the measurements conducted one and three months after the treatment we found greater pressure-lowering effect of SLT on more pigmented EG group, which is similar to Chen et al. findings, but not in the end of the follow-up. According to the results of the current study the better response to SLT in EG patients cannot be explained solely with degree of TM pigmentation.
Several studies have confirmed that SLT is an effective method of lowering IOP in POAG patients. However, the success rate (IOP reduction > 20%) varies widely from study to study. After a one-year follow-up Nagar et al. found the success rate to be 82% in patients with 360° SLT. Weinand and Althen [26] had a success rate of 60% with 180° SLT, while in the study by Saito et al. [27] study it was 23.2% in patients with 180° SLT. Prasad et al. [10] found 360° SLT to be more efficient for lowering IOP and reducing its fluctuation than 180° of treatment. Nagar et al. [4] study showed the same tendency. The possible ?dose-response? of SLT in terms of the degree of angle treated and the number of applications are used is disputable. The current study found no direct correlation between the number of laser applications and the SLT IOP-lowering effect, either in EG or in POAG groups.
To our knowledge very few prospective clinical trials have been conducted that compared the lastingness of IOP reduction of EG and POAG to SLT.
Dr. Gra?ner found the survival rate for EG patients to be 64% and 78% for POAG patients after a one-year follow-up with no significant difference between the two groups [3]. That study involved relatively small patients groups (10 patients/eyes in both groups) and it remains unclear whether logistic regression analysis were conducted separately for TM pigmentation and the presence of exfoliation material (EXM).
In general, the response rates in the present study were comparable with Gra?ner [3] study but had significantly better success rate in EG patients compared to POAG patients, (87.3% and 69.7%, respectively). Further studies are required in order to differentiate the impact of EXM for SLT outcome.
SLT is a safe method of lowering IOP in POAG and EG patients. SLT causes no thermal damage or disruption of the trabecular texture [1,18,19]. The present study did not record any visible signs of structural changes of TM or PAS formation in either group. Unlike Nagar et al. [4] no signs of severe inflammation or mild uveitis in the postoperative period were found, despite relatively high used energy. Moderate postoperative irritation and discomfort in the first few postoperative days were transient and self-limiting. Patients in both groups had no need for postoperative anti-inflammatory medications. Previous studies of SLT seem to have shown a trend toward a decreasing response of SLT with anti-inflammatory medications [21]. Realini et al. [28], however, found that topical anti-inflammatory therapy did not affect the IOP-lowering effect of SLT. This possible impact of anti-inflammatory medications to IOP needs further investigations.
Data from the present study suggests that SLT appears to be equally effective and well tolerated in EG patients. Moreover, EG patients seem to have a longer pressure-lowering effect than POAG. Hong et al. concluded in their study that repeat 360° SLT may be safe and effective after an initially successful SLT has failed. Safe, effective and potentially repeatable SLT provides additional IOP reduction in more aggressive EG cases.
References
7. Realini T (2008) Selective laser trabeculoplasty: a review. J Glaucoma 17: 497-502.