Research Article
Alexander K. C. Leung1*, Benjamin Barankin2, and Kam Lun Hon3
1Clinical Professor of Pediatrics, University of Calgary, Pediatric Consultant, Alberta Children?s Hospital
2Medical Director and Founder, Toronto Dermatology Centre
3Professor of Pediatrics, Chinese University of Hong Kong
Corresponding author
Alexander K. C. Leung, MBBS, FRCPC, FRCP (UK & Irel), FRCPCH, FAAP, Clinical Professor of Pediatrics, University of Calgary, Pediatric Consultant, Alberta Children?s Hospital, Canada, Tel: (403) 230-3322; Fax: (403) 230-3322; E-mail: aleung@ucalgary.ca
Received Date: 14thAugust 2014
Accepted Date: 10th September 2014
Published Date: 16th September 2014
Citation
Leung AK, Barankin B, Hon KL (2014) Dyshidrotic Eczema. Enliven: Pediatr Neonatol Biol 1(1): 002.
Copyright
@ 2014 Dr. Alexander K. C. Leung. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Dyshidrotic eczema, also known as dyshidrotic dermatitis or pompholyx, is characterized by pruritic, tense, deep-seated vesicles mainly on the palms and lateral surfaces of the fingers. In the chronic phase, scaling, desquamation, fissuring, and, sometimes, lichenification may be seen. The peak age of onset is between 20 and 30 years of age. The sex incidence is approximately equal. Most cases are idiopathic. Predisposing factors include atopy, contact allergens, contact irritants, dermatophyte infection, allergy to ingested metal, hyperhidrosis, prolonged use of protective gloves, intravenous immunoglobulin, psychological stress, and smoking. Although the disease is benign, it tends to run a chronic and relapsing course. Successful treatment requires a systemic multipronged approach that consists of avoidance of triggering factors, optimal skin care, pharmacotherapy during acute exacerbations, and education of patients/caregivers. Ultrapotent topical corticosteroids are the mainstay of pharmacotherapy.
Keywords :
Dyshidrotic eczema; Dyshidrotic dermatitis; Pompholyx; Pruritic vesicles; Palms; Fingers; Relapsing; Corticosteroids
Introduction
Dyshidrotic eczema, also known as dyshidrotic dermatitis or pompholyx, is characterized by pruritic, tense, deep-seated vesicles mainly on the palms and lateral surfaces of the fingers [1]. The term ?dyshidrosis? (Greek, hidrosis meaning sweat) was coined by Fox in 1873 to describe a blistering disease of the palms and soles, presumably due to a disorder of the sweat glands [2]. The term ?dyshidrosis? is a misnomer as it is now recognized that the condition has nothing to do with dysfunction of the sweat glands.
Epidemiology
The prevalence of hand dermatitis varies from 2 to 8.9% of the general population [3]. Dyshidrotic eczema accounts for 5 to 20% of all cases of hand dermatitis [4,5]. In one population study, the one-year prevalence of dyshidrotic eczema was estimated to be 0.5% [6]. Although dyshidrotic eczema occurs worldwide, it is less common among Asians [7,8]. The condition is more common in hot weather [9]. The peak age of onset is between 20 and 30 years of age [3]. Onset before 10 years of age is unusual The sex incidence is approximately equal [5].
Etiology and Pathogenesis
The exact etiology is not known. Most cases are idiopathic. Factors that may predispose to the development of dyshidrotic eczema in a susceptible individual include atopy, contact allergens, contact irritants, dermatophyte infection, allergy to ingested metal (in particular, nickel and cobalt), hyperhidrosis, prolonged use of protective gloves, intravenous immunoglobulin, psychological stress, and smoking [4,8,10-12]. Most cases are sporadic. Rarely, an autosomal dominant mode of inheritance has been described [5]. A gene locus on chromosome 18q22.1-18q22.3 was identified in a large Chinese family with 14 affected individuals through 4 generations [5].
Histopathology
In the acute phase, histologic features include intraepidermal spongiosis with vesicle formation and a superficial perivascular inflammatory infiltrate composed mainly of lymphocytes and histiocytes [3,4,11,12]. In the more chronic phase, there are multiple foci of parakeratosis, acanthosis, irregular epidermal hyperplasia with minimal or absent spongiosis [3,4,12]. The epidermis is thick and the overlying horny layer is even thicker [8].
Clinical Manifestations
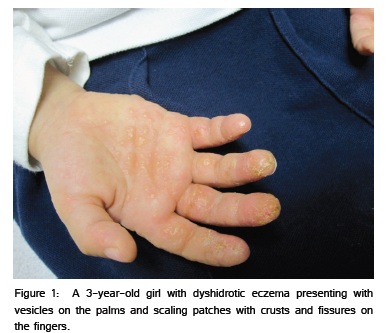
Clinically, acute dyshidrotic eczema presents with a sudden outbreak of deep-seated ?tapioca-like? vesicles and, less commonly, bullae that affect primarily the palms and lateral surfaces of the fingers [1,9]. The eruption may also occur on the soles of the feet. In approximately 80% of cases, only the hands are affected [4]. The eruption is usually symmetrical and pruritic [1]. Some patients experience pain and/or a burning sensation [1]. In the chronic phase, scaling, desquamation, fissuring, and, sometimes, lichenification may be seen [1]. The condition is typically recurrent and both the acute and chronic phases can coexist (Figure 1).
Diagnosis and Differential Diagnosis
The diagnosis is mainly clinical based on a detailed history and the appearance of the rash. Differential diagnosis includes allergic contact dermatitis (can be determined by patch testing to various contactants), irritant contact dermatitis (typically over-washing, using harsh soaps and/or insufficient moisturizing) , and atopic hand dermatitis (typically a family or personal history of eczema, asthma, and/or hay fever) most commonly; much less commonly, the differential would include epidermolysis bullosa simplex, bullous impetigo, herpes infection, id reaction, linear IgA disease, dyshidrotic tinea, dyshidrosiform pemphigoid, pemphigus vulgaris, fixed drug eruption, acropustulosis of infancy, hand-foot-mouth disease, pustular psoriasis, palmoplantar pustulosis, secondary syphilis, and acrodermatitis enteropathica [8,12].
Complications
Dyshidrotic eczema has a significant negative impact on the quality of life due to the severe pruritus [5,9]. Secondary bacterial infection, especially with Staphylococcus aureus, is not uncommon [4]. Nail dystrophy may result if the nail matrix is affected [4].
Prognosis
Although the disease is benign, it tends to run a chronic and relapsing course [3]. The condition tends to be less severe and recurs less often with age [4]. Most patients eventually outgrow the condition [4].
Management
Dyshidrotic eczema is often difficult to treat, possibly because of the thick epidermis with a compact stratum corneum and richness of the sweat glands of the affected skin. Successful treatment requires a systemic multipronged approach that consists of avoidance of triggering factors, optimal skin care, pharmacotherapy during acute exacerbations, and education of patients/caregivers.
Soaps and detergents should be avoided as much as possible [13]. The hands should be washed with lukewarm (not hot) water and soap free cleansers. Emotional stress often exacerbates the skin lesions of atopic dermatitis. If avoidance is not possible, coping mechanisms should be tried [13].
Hydration of the skin helps to improve the dryness and pruritus and restore the disturbed skin?s barrier function. As such, hydration of the skin is of paramount importance both in the prevention and management of dyshidrotic eczema. A moisturizer or emollient should be applied as soon as possible after hand-washing to prevent evaporation of water and to keep the skin soft and flexible. In general, ointments are most effective but messy; creams are often better tolerated. The type of moisturizer or emollient should be tailored to the individual skin conditions as well as the child?s needs and preferences [13].
Ultrapotent topical corticosteroids are the mainstay of therapy. Topical corticosteroids should not be applied more than twice a day; frequent use does not improve efficacy and increase the risk of side effects [14]. Topical immunomodulators such as tacrolimus and pimecrolimus are not as fast or effective as ultrapotent topical corticosteroids in the treatment of this skin condition, although they can be considered in the maintenance phase of treatment [4]. Both topical steroids and immunomodulators are commonly and safely used in children [4]. Systemic corticosteroids should be reserved for recalcitrant cases and used for the shortest time possible (typically 1 week or so) while awaiting response to other therapies. Other immunosuppressants such as cyclosporine, azathioprine, and methrotrexate have occasionally be used for recalcitrant and severe cases unresponsive to the above measures, but with variable success, and typically not in children [8]. These immunosuppressants all have potential adverse effects, requiring careful monitoring and restricting their clinical usefulness [13]. Psoralen plus ultraviolet A (PUVA), UVA1 and UVB have been shown to be effective and may be considered in the treatment of refractory cases in older children [8]. Narrow-band UVB is most commonly used. More recently, oral alitretinoin has been shown to be effective for recurrent and refractory cases of this condition in adults. The response rate is approximately 50% [15].
Intradermal botulinum toxin A has also been tried with some success in patients with concomitant hyperhidrosis [16]. The medication has potent antihidrotic activity [16]. Since hyperhidrosis is an aggravating factor, treatment of hyperhidrosis may lead to regression of the disorder. The drawback is the need for repeated injections approximately every 6 months. This is rarely used in children because of the pain involved.
Although pruritus in dyshidrotic eczema does not appear to be mediated by histamine release, oral antihistamines can provide symptomatic relief because of their sedative properties and may be effective for intense pruritus refractory to moisturizers and conservative measures. Of the H1 antihistamines, hydroxyzine is more effective than diphenhydramine and cyproheptadine [13].
Patient/caregivers education and support are vital in the management of dyshidrotic eczema. Misinformation may be detrimental to disease control. Steroid fear or phobia among patients/caregivers is common and is a significant factor in suboptimal use or non-compliance to treatment [17]. Poor compliance is a major reason for treatment failure. Patients and caregivers should be reassured that topical corticosteroids are safe and effective with their sensible use and they remain first-line treatment for acute flares [17].
References
2. Fox T (1873) Clinical lecture on Dyshidrosis: an undescribed eruption. Br Med J 2: 365-366.
7. Lee CS, Lim HW (2003) Cutaneous diseases in Asians. Dermatol Clin 21: 668-677.
14. Baumer JH (2008) Atopic eczema in children, NICE. Arch Dis Child Educ Pract Ed 93: 93-97.