Case Report
Delayed Intractable Postextubation Laryngeal Edema after General Anesthesia
Kyung Woo Kim, MD1, Ji Yeon Kim, MD, PhD2*, Jun Hyun Kim, MD2, Min Hee Heo, MD2, Sang-il Lee, MD2, Kyung-Tae Kim, MD, PhD2, Won Joo Choe, MD, PhD2, Jang Su Park, MD, PhD2, and Jung Won Kim, MD, PhD2
1Anesthesiology and Pain Medicine, Inje University Seoul Paik Hospital
2Anesthesiology and Pain Medicine, Inje University Ilsan Paik Hospital
Corresponding author
Ji Yeon Kim, MD, PhD, Inje University, Ilsan Paik Hospital, 2240 Daehwa-dong, IlsanSeo-gu, Goyang-si, Gyeonggi-do, Korea, Tel: 82-31-910-7187; Fax: 82-31-910-7184; E-mail: jy67925@naver.com
Received Date: 21 March 2014
Accepted Date: 06 April 2014
Published Date: 10 April 2014
Citation
Kim KW, Kim JY, Kim JH, Heo MH, Lee SI, et al. (2014) Delayed Intractable Postextubation Laryngeal Edema after General Anesthesia. Enliven: J Anesthesiol Crit Care Med 1(1): 005.
Copyright
@ 2014 Dr. Ji Yeon Kim. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, that permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
We report a case of delayed intractable postextubation laryngeal edema after extubation in 78-year-old female patient who underwent uneventful operation. The patient had underwent tracheostomy 30 years ago. After 14 hours extubation, she developed postextubation laryngeal edema. Reintubation was done, and she was transferred to the intensive care unit. After this, tracheal intubation is repeated, postextubation laryngeal edema occurs again 48 hours after extubation the last, after all, the patient underwent a tracheostomy. postextubation laryngeal edema can happen any time after the extubation despite of intensive treatment, particularly in patients with history of previous tracheostomy. It seems ideal to avoid tracheal manipulation if other anesthetic plan is available and careful history taking and evaluation of airway will be helpful for these patients.
Keywords
Airway management; Airway obstruction; Laryngeal edema; Steroids; Tracheal extubation
Abstract
We report a case of delayed intractable postextubation laryngeal edema after extubation in 78-year-old female patient who underwent uneventful operation. The patient had underwent tracheostomy 30 years ago. After 14 hours extubation, she developed postextubation laryngeal edema. Reintubation was done, and she was transferred to the intensive care unit. After this, tracheal intubation is repeated, postextubation laryngeal edema occurs again 48 hours after extubation the last, after all, the patient underwent a tracheostomy. postextubation laryngeal edema can happen any time after the extubation despite of intensive treatment, particularly in patients with history of previous tracheostomy. It seems ideal to avoid tracheal manipulation if other anesthetic plan is available and careful history taking and evaluation of airway will be helpful for these patients.
Tracheal intubation always has a risk of laryngotracheal injury and the possibility of laryngeal edema due to laryngotracheal injury [1]. Postextubation laryngeal edema (PLE), which could take place immediately after an extubation, makes airway management difficult. Reintubation may causes prolonged mechanical ventilation and an increased length of stay in the intensive care unit as well as an increased mortality [2]. The percentage of PLE occurrence is about 2-22%. PLE mainly occurs within 30 minutes after extubation regardless of the severity of symptoms. Forty-seven percent of PLE cases occur within five minutes [3].
Herein, with relevant references, we report a case of PLE that first occurred 14 hours after extubation and again 48 hours after the extubation even though many treatment methods were used in the intensive care unit after the initial PLE.
Case Report
A 78-year-old female patient, with a height of 150 cm and a weight of 54 kg, was admitted with a right femur intertrochanteric fracture; thus, surgery under general anesthesia was planned. The patient had undergone a tracheostomy 30 years ago during treatment for carbon monoxide gas poisoning. The tracheostomy site was fully healed. In the preoperative evaluation, the chest x-ray analysis showed cardiomegaly, but there were no other abnormalities.
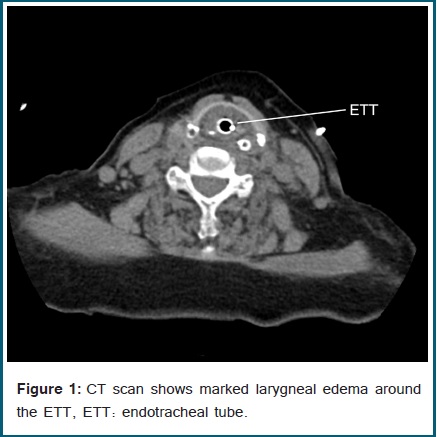
The preanesthetic vital signs were normal. The anesthetic induction was performed with propofol, remifentanil, and rocuronium, and the anesthesia was maintained with remifentanil and desflurane. The Cormack-Lehane classification was Grade 2. A 7.0 cuff endotracheal tube was inserted without any difficulties or resistance during the intubation. The surgery was finished within two hours. Extubation was performed after recovery of spontaneous breathing without any particular events. The patient was moved to the recovery room and then to the ward. There were no abnormalities in breathing. A little wheezing was heard in the upper airway four hours after the surgery. The peripheral vascular arterial oxygen saturation (SaO2) was 92% in room air, but the patient did not complain of respiratory distress. Administration of nasal prong O2 1 L/min was started. Salbutamol (Ventolin Nebule®, GlaxoSmithKline plc., Brentford, UK) and Ipratropium Br (Atrovent UDV®, Boehringer Ingelheim, Seoul, Korea) were nebulized. Then, the SaO2 increased to 95%, so the patient was closely monitored. Ten hours after that, the patient suddenly complained of respiratory distress, and the SaO2 was decreased to 88%. Although oxygen administration was increased, the SaO2 decreased and wheezing increased. An emergent airway intubation was performed. When a 6.0 cuff endotracheal tube was inserted, there was a little resistance. Then, the patient was transported to the intensive care unit. Because airway edema was suspected, Budesonide (Pulmicort Respules®, AstraZeneca AB, Södertälje, Sweden) 0.25 mg and Ipratropium Br 250 mcg were nebulized four times a day. Methylprednisolone sodium succinate (Solu Medrol®, Pfizer Korea, Seoul, Korea) 40 mg was intravenously injected once a day. The SaO2 was maintained at about 94% in room air. A negative result was found in the cuff-leak test 36 hours after the intubation; thus, extubation was performed. After the extubation, 5 mg of dexamethasone (Dexamethasone®, YuhanMedica, Cheongwon, Korea) was intravenously injected. Nasal prong O2 3 L/min was administered, and the SaO2 was maintained at 95-100%. However, a second intubation was performed because respiratory distress and decreased SaO2 was observed 48 hours after the first extubation. A neck CT performed after the intubation showed laryngeal edema (Figure 1).
To reduce the airway edema, methylprednisolone sodium succinate 40 mg was intravenously injected every six hours. Because the airway edema was decreased on the fourth day after the reintubation, extubation was planned. On the fourth day after the reintubation, dexamethasone 5 mg/bid was intravenously injected, and extubation was performed on the fifth day after intravenously injecting dexamethasone 2.5 mg. After the extubation, dexamethasone 5 mg was intravenously injected once again. A mixed solution of Epinephrine HCl (Bosmin®, Jeil Pharmaceutical Co., Ltd, Seoul, Korea) 2 cc and N/S 3 cc was nebulized four times in a one-hour interval. After the extubation, SaO2 was maintained at about 94 % without respiratory distress. However, two days later, respiratory distress and decreased SaO2 occurred again. By increasing the inhalation oxygen concentration, injecting dexamethasone 5 mg intravenously, and nebulizing epinephrine, pH 7.5, PaCO2 29.2, PaO2 55.6, and SO2 92.2% were maintained with a high flow FiO2 of 0.45. Accompanying pneumonia was found. Because steroid administration was difficult to maintain further due to the pneumonia and inflammation at the operated region, tracheostomy was decided. Fourteen days after the tracheostomy, the pneumonia was resolved, and the patient was discharged from the intensive care unit.
Discussion
PLE is a common cause of airway obstruction after extubation. PLE is caused by ulceration at the posterior to the level of the vocal cord where the endotracheal tube is located and by damage to the laryngeal mucosa layer due to pressure and ischemia by generation of granulation tissue [4].
In the treatment of PLE, a rapid and early detection of PLE is most important above all else. The therapeutic regimen includes inhalation or intravenous steroid administration and epinephrine aerosol inhalation [4]. It has been reported in many previous studies that the administration of a steroid could prevent PLE [3,5]. The initial anti-inflammatory effects of steroid administration start within 1-2 hours after the intravenous injection and reach a maximum in 2 to 24 hours [6].
Therefore, the timing and administration method are important in the steroid treatment. Neither the pretreatment of a steroid provided one hour before the extubation nor the administration of hydrocortisone 100 mg was effective against postextubation stridor (PES) or PLE [7]. A PLE prevention effect was found in a regimen in which a total of 20 mg of dexamethasone was administered from the time 24 hours before the planned extubation, four times at 5 mg each time, every six hours after that [5], and in a regimen in which a total of 160 mg of methylprednisolon was intravenously injected from the time 24 hours before the planned extubation to every six hours after that [8]. The purpose of such a multiple-dose regimen is to take advantage of the fact that an early start of steroid treatment and repeated administration of the drug at each of the half-life times have shown a high level anti-inflammatory effect and limited mucosa layer edema after extubation [9]. Although a standard steroid regimen for prevention of PLE has not been determined, most reports have shown that it is appropriate to intravenously inject methylprednisolone 20-40 mg from the time 12 to 24 hours before an extubation to every four to six hours after that [10].
In the treatment of PLE by epinephrine nebulization, racemic epinephrine, which is a mixture of the two isomers, is used because racemic epinephrine shows more continuous and stable effects than those of L-form epinephrine alone [11]. However, the use of L-form epinephrine for PLE treatment may be appropriate because the pharmacologic action of racemic epinephrine is mostly from the L-isomer, and the L-form is easy to obtain and low in price, showing an equivalent effect compared to the racemic epinephrine [12]. Although epinephrine decreases inflammatory exudates and edema by causing a decrease in the pre-capillary and post-capillary pressure through a vasoconstriction effect, a combined administration of epinephrine and dexamethason did not show any effect of decreasing edema because the PLE induced by ischemia and inflammatory exudates is a more intense edema than that of a laryngeal edema induced by other causes and thus, is more resistant to the effect of epinephrine [13].
In this reported case, wheezing without respiratory distress was heard four hours after the surgery, and so the patient was closely monitored. A PLE requiring reintubation occurred 14 hours after the surgery. Later, even in the intensive care unit, a PLE occurred once again 48 hours after the surgery. In this case, although steroid administration and epinephrine nebulization were performed as treatments, long-term steroid administration could not be maintained because of pneumonia and continued inflammation at the operated region
In addition, because the symptoms did not rapidly improve due to the base stenosis at the previous tracheostomy site, a tracheostomy was unavoidably performed. Although most PLE-related stridor cases take place in the inspiratory phase, an expiratory stridor was found at a sternal notch site in our case. The expiratory stridor might have occurred because of granulation tissue which was found during the tracheostomy. In that situation, a tiny subglottic stenosis was already there because of a tracheostomy that the patient had previously undergone. It is presumed that the granulation tissue of the patient might have been generated by several steps of inflammation reactions which were caused by direct mechanical trauma from a few attempts of intubation after the first PLE.
One unsatisfactory feature of the management of the patient was that an appropriate dose of steroid was not administered to the patient from the time of the initial generation of the PLE. Although a steroid at a higher dose than the previous one was administered after the second reintubation, PLE took place 48 hours later. In a patient with a past history of tracheostomy, as in this case, inflammatory edema caused by laryngotracheal injury related to intubation could have exacerbated the existing airway stenosis. Therefore, an early and proactive steroid administration could have mitigated the continued PLE through the anti-inflammatory effect of the steroid.
In conclusion, although a careful observation during the first hour after extubation is important in a patient who may develop PLE [13], as in this case, it should be recognized that PLE could take place even some time after extubation and even after the patient has undergone intensive care. In addition, a patient’s medical history should be carefully examined, and the airway should be evaluated carefully. In patients with a past history of tracheostomy, different anesthetic methods may need to be considered depending on the types of surgery so that airway manipulation could be avoided if possible. When performing general anesthesia with such patients having a past history of a tracheostomy, the size of the endotracheal tube should be chosen carefully. In addition, efforts should be made to reduce the PLE incidence by performing early pretreatment administration of steroids at the appropriate time and with an appropriate dose. The patient agreed to have her case presented to the public for academic purposes
Declaration
The authors declare that they have no competing interests.