Research Article
Cuffed Endotracheal Tube Size and Leakage in Pediatric Tracheal Models
Jun Hyun Kim1, Kyung Woo Kim2, Heo Min Hee1, Sang-il Lee1, Ji Yeon Kim1, Kyung-Tae Kim1, Jang Su Park1, Jung Won Kim1, and Won Joo Choe1*
1Anesthesiology and Pain Medicine, Inje University Ilsan Paik Hospital
2Anesthesiology and Pain Medicine, Inje University Seoul Paik Hospital
Corresponding author
Won Joo Choe, MD, PhD, Inje University Ilsan Paik Hospital, 2240 Daehwa-dong, IlsanSeo-gu, Goyang-si, Gyeonggi-do, Korea, Tel: 82-31-910-7185; Fax: 82-31-910-7184; E-mail: humal1@paik.ac.kr
Received Date: 11 March 2014
Accepted Date: 12 April 2014
Published Date: 16 April 2014
Citation
Kim JH, Kim KW, Kim JH, Hee HM, Lee SI, et al. (2014) Cuffed Endotracheal Tube Size and Leakage in Pediatric Tracheal Models. Enliven: J Anesthesiol Crit Care Med 1(1): 006.
Copyright
@ 2014 Dr. Won Joo Choe. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, that permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Object:
Cuffed endotracheal tubes are increasingly used in pediatric patients in the hope that they can reduce air leakage and tube size mismatch by just inflating the cuff. Authors compared influence of various tube sizes and different levels of cuff pressures to air leakage around the cuff, in artificial tracheal models.
Methods:
Six PVC cylinders of different internal diameters (ID: 8.15, 8.50, 9.70, 12.05, 14.50, and 20.00 mm) were prepared. An artificial lung connected with cylinder was ventilated with an anesthesia machine. Cuffed endotracheal tubes of different sizes (ID 3.0~8.0) were located in the cylinders and the cuff was inflated with various pressures (15, 20, 25, 30 and 35 cm H2O). Expiratory tidal volume was measured with more than 25% loss of baseline expiratory tidal volume was considered significant air leakage.
Results:
Tube sizes same as, or larger than ID 5.0 didn’t show significant air leakage for any trachea model, only if the inflated cuff size is larger than the cylinder ID, except ID 5.5 tube at cuff pressure 15 cm H2O and 20 cm H2O, in 12.05 mm cylinder. Tubes sizes same as or smaller than ID 4.5, which have short cuff lengths and sizes than tubes larger than, or same as ID 5.0, leaked significantly at any tracheal models, except ID 4.5 tube at cuff pressure 35 cm H2O, in 8.50 mm cylinder.
Conclusion:
In PVC pediatric tracheal models, tubes same as, or smaller than ID 4.5 are inferior to tubes same as, or larger than ID 5.0 in preventing air leakage, and may need a higher cuff pressure to reduce air leakage. Further clinical studies could be designed based on our results.
Keywords
Airway management; Child; Endotracheal; Devices; Intubation; Trachea
Abstract
Object: Cuffed endotracheal tubes are increasingly used in pediatric patients in the hope that they can reduce air leakage and tube size mismatch by just inflating the cuff. Authors compared influence of various tube sizes and different levels of cuff pressures to air leakage around the cuff, in artificial tracheal models.
Methods: Six PVC cylinders of different internal diameters (ID: 8.15, 8.50, 9.70, 12.05, 14.50, and 20.00 mm) were prepared. An artificial lung connected with cylinder was ventilated with an anesthesia machine. Cuffed endotracheal tubes of different sizes (ID 3.0~8.0) were located in the cylinders and the cuff was inflated with various pressures (15, 20, 25, 30 and 35 cm H2O). Expiratory tidal volume was measured with more than 25% loss of baseline expiratory tidal volume was considered significant air leakage.
Results: Tube sizes same as, or larger than ID 5.0 didn’t show significant air leakage for any trachea model, only if the inflated cuff size is larger than the cylinder ID, except ID 5.5 tube at cuff pressure 15 cm H2O and 20 cm H2O, in 12.05 mm cylinder. Tubes sizes same as or smaller than ID 4.5, which have short cuff lengths and sizes than tubes larger than, or same as ID 5.0, leaked significantly at any tracheal models, except ID 4.5 tube at cuff pressure 35 cm H2O, in 8.50 mm cylinder.
Conclusion: In PVC pediatric tracheal models, tubes same as, or smaller than ID 4.5 are inferior to tubes same as, or larger than ID 5.0 in preventing air leakage, and may need a higher cuff pressure to reduce air leakage. Further clinical studies could be designed based on our results.
Introduction
In the past, for the pediatric population, uncuffed endotracheal tubes were thought to be ideal for airway management. But usage of cuffed endotracheal tubes in pediatric patients is increasing, and evidences are showing that a cuffed tube does not cause more airway injury than an uncuffed tube [1-3]. Cuffed tubes are thought to be superior to uncuffed tubes in reducing air leakage. Reducing leakage volume is crucial for properly confirm intended tidal volume and pressure are delivered [4]. Excessive air leakage around the tube can cause unnecessary tube changes, reintubation, and airway injuries.
But, sometimes, it is difficult to prevent air leakage even when a cuffed tube is used. We experienced some cases in which carefully chosen cuffed endotracheal tubes leaked even at significantly high cuff pressures. And several researches about choosing right sized cuffed endotracheal tubes for pediatric patients didn’t show consistency among them [5,6].
Because of inconsistency of reports about choosing suitable sizes of cuffed endotracheal tubes, we designed this preliminary bench-top study to evaluate various tube sizes and cuff pressures at once. We used PVC cylinders, although they have many limitations compared to real tracheae. We evaluated various sizes of tracheal models, endotracheal tubes, and cuff pressures to find out the optimal size of tube and cuff pressure to minimize air leakage.
Methods and Materials
We prepared six PVC cylinders which have different internal diameters of 8.15, 8.50, 9.70, 12.05, 14.50, and 20.00 mm. These cylinders were made out of different sizes of syringes, cutting off both ends. Internal diameters were measured three times by vernier caliper and averaged. These internal diameters are accounting for the internal diameters of the trachea for ages of 3, 4, 8, 12, 16, and adults, respectively, according to Griscom and Wohl’s data [7].
The authors prepared adult and pediatric breathing bags as artificial lungs and a ventilator. Ventilator (Aestiva 3000™, Datex-Ohmeda, Madison, WI, USA) was set to an air flow of 4 liters per minute and an oxygen flow of 4 liters per minute. The pediatric breathing bag directly connected to the ventilator via a pediatric corrugated circuit (Acemedical, Seoul, Korea) and ventilator was set to the tidal volume (TV) of 250 ml, respiratory rate (RR) of 20 per minute, expiratory pause time of 25%. It showed a peak inspiratory pressure (PIP) of 23 cm H2O, a plateau pressure (Ppl) of 23 cm H2O, and an expiratory volume (TVexp) of 233 ml. This expiratory volume was used as a baseline to calculate air leakage for pediatric lung model. The adult breathing bag connected via an adult corrugated circuit to the same ventilator and it was set to a TV of 500 ml, an RR of 12 per minute, and showed a PIP of 21 cm H2O Ppl of 19 cm H2O and a TVexp of 460 ml. This expiratory volume was used as a baseline value for adult lung model.
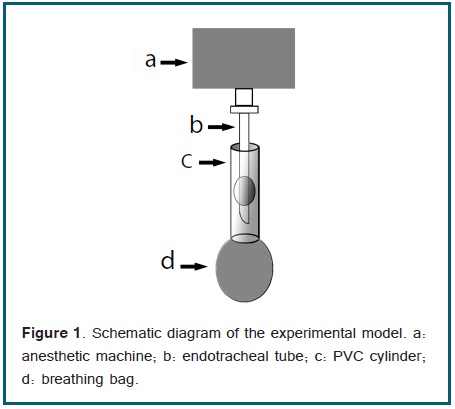
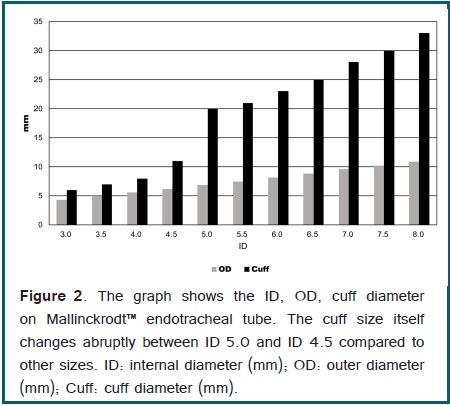
Four cylinders with smaller diameters (8.15, 8.50, 9.70, and 12.05 mm) were connected to pediatric breathing bag. Two cylinders with larger diameters (14.50 and 20.00 mm) were connected to the adult breathing bag. Then we connected an endotracheal tube to the ventilator and carefully located the tube cuff at the center of the cylinder (Figure 1). We used ID 5.0 ~ ID 8.0 Mallinckrodt™ Hi-Lo and ID 3.0 ~ ID 4.5 Mallinckrodt™ Hi-Contour tracheal tubes (Covidien, Mansfield, MA, USA). Reported internal diameter, outer diameter and cuff diameter by the manufacturers are shown in Figure 2.
Each cylinder and breathing bag was connected using elastic rubber strips wrapped around the cylinder until it fitted into breathing bag. Air leakage was checked by auscultation and bag test. We used Trachoe® (TRACOE medical GmbH, Frankfurt, Germany) to measure and set the cuff pressure. We disconnected it from the cuff before starting mechanical ventilation to prevent a PIP higher than cuff pressure resulting in loss of cuff pressure in expiratory phase. The cuff was filled with room air. We changed cuff pressure from 15 cm H2O to 35 cm H2O, at 5 cm H2O intervals. After starting mechanical ventilation, we waited until the TVexp difference between each breath became less than 5 ml, then a mean TVexp of six consecutive breaths was recorded.
We defined significant air leakage as a TVexp smaller than 75% of the baseline TVexp. We measured air leakages using six new tubes at each size, at five different cuff pressures. Data were analyzed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA). Mann-Whitney rank sum test was used. A one-tailed p value of < 0.05 was considered statistically significant
Results
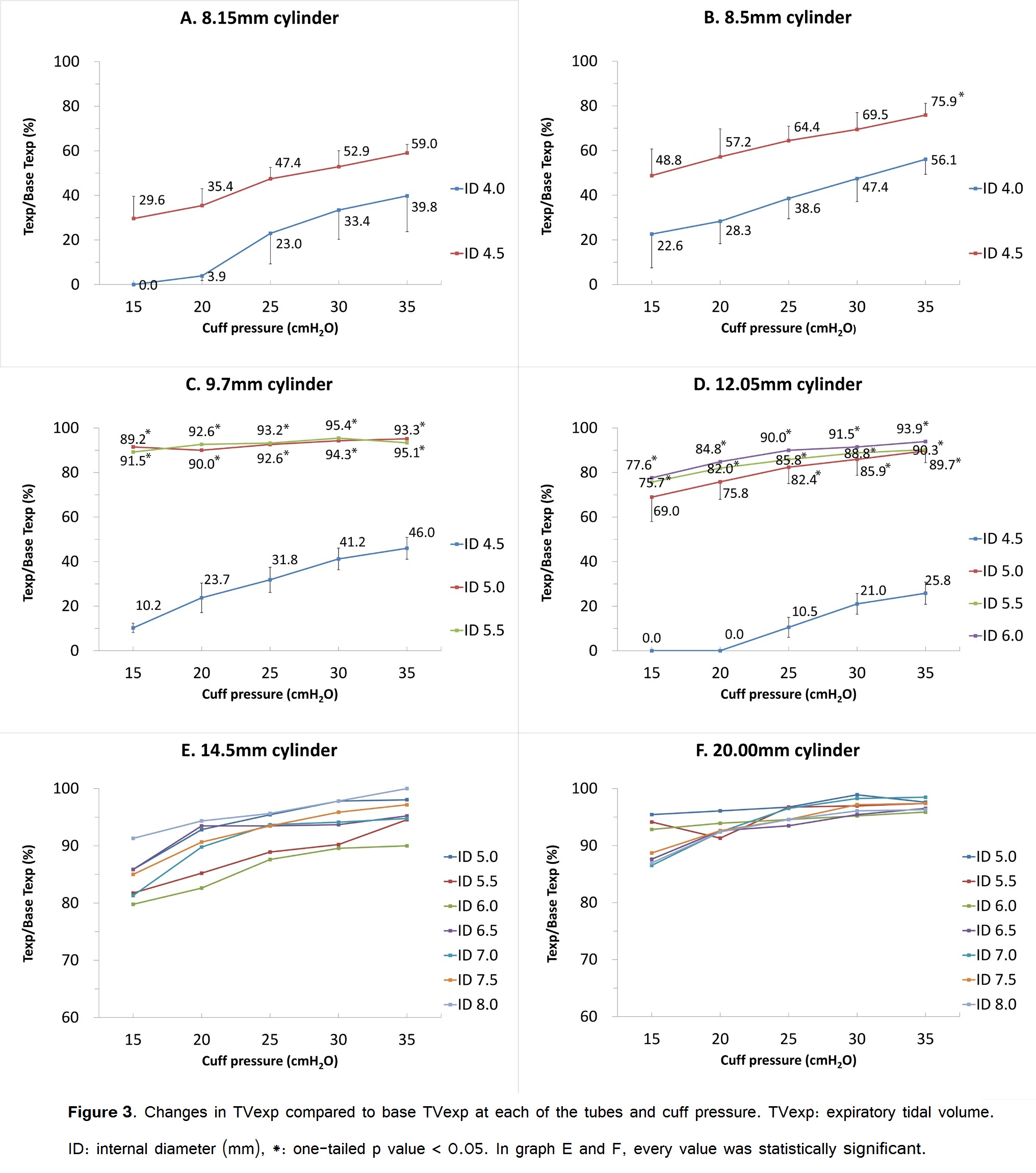
We presented reduced expiratory volume percent compared to base TVexp at each of the tubes, cuff pressures in Figure 3. Relationships between model tracheae, recommended tube sizes, and leakages are presented in Table 1. A 8.15 mm model trachea represents the trachea of approximately a 3 years old child.
The optimal tube size for this trachea size by Khine’s formula [5] is 3 years/4 +3, and therefore is 4. By Duracher’s formula [6], it is 4.5. ID 4.0 and ID 4.5 tubes showed significant leakage at all cuff pressure levels. ID 5.0 tube was not able to be inserted into the model trachea, because of the cuff frill.
| Cylinder Diameter | Age* | Suitable tubes† | Results |
|
8.15 mm |
3 |
ID 4.0 or 4.5 |
Leaked at all cuff pressures. |
|
8.50 mm |
4 |
ID 4.0 or 4.5 |
ID 4.0 leaked at all pressures. |
|
9.70 mm |
8 |
ID 5.0 or 5.5 |
Both prevented leakage. |
|
12.05 mm |
12 |
ID 6.0 or 6.5 |
ID 6.0 prevented leakage. |
|
14.50 mm |
16 |
ID 7.0 or 7.5 |
Both prevented leakage. |
|
20.00 mm |
adult |
|
ID 5.0-8.0 prevented leakage. |
* Corresponding age by trachea diameter according to Griscom and Wohl’s [7] data
† Suitable tube sizes calculated by Khine et al’s formula[5] and Duracher et al’s formula [6], respectively.
An 8.50 mm model trachea represents a 4 years old child. By Khine’s formula, the suitable tubes is ID 4.0, and by Duracher’s, it is ID 4.5. The ID 4.0 tube had smaller cuff diameter (which is 8 mm) than the cylinder, and it leaked significantly at any cuff pressure levels. An ID 4.5 tube had enough cuff diameter (which is 11 mm) to seal the cylinder, but it leaked significantly until cuff pressure reached 30 cm H2O (Figure 3B). It was impossible to put in an ID 5.0 or 5.5 tube in this cylinder, because of the deflated and frilled cuffs. Because of this we were not able to test an ID 5.0 or 5.5 tube in this model. A 9.70 mm model trachea represents an 8 years old child. By Khine’s formula, the suitable tube size is ID 5.0 and by Duracher’s, it is ID 5.5. Both tube was able to ventilate the artificial lung without significant air leakage. The ID 4.5 tube (which has 11 mm cuff diameter) leaked significantly although it had enough diameter to seal the cylinder. ID 6.0 or larger tubes couldn’t be put in this cylinder, because of the cuff frill.
A 12.05 mm model trachea represents a 12 years old child. By Khine’s formula, the suitable tube size is ID 6.0, by Duracher’s it is ID 6.5. It was not possible to insert the ID 6.5 or larger tubes into the cylinder because deflated cuff made frills. Tube sizes of ID 6.0 to 5.0 prevented air leakage at any pressure levels, except ID 5.0 tube at 15 cm H2O and 20 cm H2O pressure.
A 14.50 mm model trachea represents a 16 years old child. By Khine’s formula, the suitable tube is ID 7.0, by Duracher’s, it is ID 7.5. All the tubes from ID 5.0 to 8.0 effectively prevented air leakage, at all cuff pressure levels. A 20.00 mm model trachea represents the trachea of an adult. All the tubes from ID 5.0 to 8.0 effectively prevented air leakage at less than 25% of TVexp.
In summary, tube size equal to or larger than ID 5.0 generally was adequate for any size of trachea model if the inflated cuff size is larger than the ID of the cylinder. But tube sizes same or smaller than ID 4.5 had some difficulties in sealing the cylinders and leaked significantly.
Discussion
Cuffed endotracheal tubes are becoming widely used in infants and small children. They are thought to be superior to uncuffed tubes at preventing air leakage, and reducing unnecessary laryngoscopic manipulation of the larynx by reducing tracheal tube size mismatch. It also has been suggested as a better option for pediatric burn patients, in regards to airway edema after an inhalation injury [8].
There were several in vivo and in vitro studies about air leakage or fluid leakage around the cuff [3,9-11]. But There have been no reports of testing different sizes of tubes on several model tracheas, at different levels of cuff pressure, that we know of.
Our results show that there are difficulties in preventing air leakage, when using endotracheal tubes smaller than ID 4.5. For example, for 8.15 mm model trachea, suitable tubes by both formulae were ID 4.0 and ID 4.5, respectively. ID 4.0 had smaller cuff diameter (which is 8 mm) than the cylinder. ID 4.5 had enough cuff diameter (which is 11 mm) to seal the cylinder, but it leaked significantly. With ID 4.5 tube, we intentionally raised cuff pressure beyond 35 cm H2O, to see if it can prevent leakage or not at any cuff pressure. Increasing cuff pressure up to 100 cm H2O eventually reduced leakage to 16.3%, but at the pressure of 45 cm H2O, leakage was more than 30% (results not reported). In other words, both tubes suggested by two formulae leaked at reasonable cuff pressure levels.
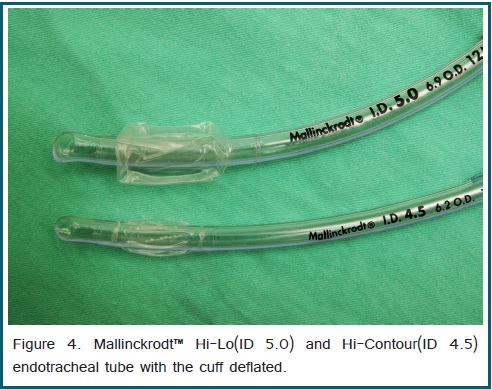
There can be several reasons for these results. First, small sized tubes inevitably have a shorter cuff length and diameter. This reduces the contact surface of the cuff and model trachea, and could be one reason for the air leakage. However, this phenomenon doesn’t seem to be significant until the ID reaches 5.0. But for ID 4.5 or smaller tubes, it becomes evident. We thought that it was caused by the change of the cuff’s design. For Mallinckrodt™ Hi-Lo tracheal tubes, ID 5.0 was the smallest one. Below the size of ID 5.0, there are only Mallinckrodt™ Hi-Contour tracheal tubes. Hi-Lo and Hi-Contour tubes are different in cuff design, which means Hi-Lo has a bigger, more rectangular cuff (when inflated), and Hi-Contour has smaller, more elliptical (or circular) cuff. The cuff size itself changes abruptly between ID 5.0 and ID 4.5, compared to other sizes (Figure 2). If the cuff design is an important factor in preventing air leakage, then it seems reasonable that all cuff design should be rectangular. But there are some reasons preventing it. Pediatric patients have a shorter trachea, which means the distance between carina and vocal cords is not long enough. If the cuff length increases, the risk of blocking the bronchus with cuff, the risk of endobronchial intubation, or risk of placing the cuff in the larynx increases, too [3]. And the more rectangular cuff design forms frills when deflated (Figure 4). The frill interfered with tube insertion and actually made it impossible to test it in our experiment, although it has outer diameter smaller than model trachea. (ID 5.0 tube in 8.15 and 8.50 mm cylinder, ID 5.5 tube in 8.15 and 8.50 mm cylinder, ID 6.0 tube in 9.70 mm cylinder, and ID 6.5 tube in 12.05 mm cylinder) And there is a report that abundance of cuff can form sharp edges when actively deflated, and can cause laryngeal damage [9].
Several studies suggest that longitudinal channels or folds formed after inflating the cuff in trachea are one of major factors contributing to post pharyngeal secretion aspiration [10,11]. Thus one can postulate that a large cuff diameter compared to the tracheal internal diameter may result in more air leakage. In 8.15 mm and 8.50 mm trachea models, ID 4.0 and 4.5 tubes both showed less leakage in larger trachea model. This may be a result of longitudinal fold formed by abundant cuff and consistent with our assumption. But for tubes larger than ID 5.0, regardless how large the cuff diameter was, if only it is big enough to seal the trachea and small enough to put in, air leakages between cuff sizes were not different significantly. In tubes same size or smaller than ID 4.5, cuff design of smaller contact surface with tracheal wall may prone to form channels which pass through the cuff, and in tubes same size or larger than ID 5.0, large contact surface with tracheal wall made channels prone to be interrupted in between. We used two formulas to predict tube sizes. According to our results, for trachea model of 3 and 4 years old child (model trachea ID of 8.15 and 8.50 mm), Duracher’s formula was more suitable to minimize air leakage.
For 8 years old child model (ID of 9.70 mm) both formula was suitable. For 12 years old child model (ID of 12.05 mm) Khine’s formula was more ideal because tube size suggested by Durachers’s formula could not be inserted due to frill. There were some limitations in our study. First of all, the trachea model was not a real trachea. It may have been possible but not ethical to evaluate several tubes and cuff pressures in actual patients. And animal trachea model would be deformed during the experiment which includes multiple manipulations and inflations, and would result in inconsistent results. A PVC cylinder doesn’t have any elasticity or mucosa. In an actual trachea, air leakage can be less than our results. Also our model had a circular cross section, but a real trachea has a flat posterior surface. We do not know circular model will leak more than actual trachea or not, but we think the leakage difference between two will not be large and the proportional changes of leakage between diameters will be the same.
Although our study is dealing with model tracheae, our results can be used as a preliminary data for study of actual human tracheae. As we mentioned, it is not easy to predict actual trachea size in children, and it is not ethical to change tubes several times in one child. With our results, future studies in human can be designed more safely. And our model may be useful in the research to reduce post pharyngeal secretion aspiration and ventilator associated pneumonia.
In regards to our study results, clinicians should be careful when choosing tubes smaller than ID 4.5, because it is not easy to predict the actual trachea size by age, also even if we know the actual trachea size, there is a fairly narrow margin of selecting the correct sized tube. A novel methods such as using ultrasonography could be a breakthrough [12,13]. We recommend, when it is possible, using tubes larger than ID 5.0. But there can be cases where the frill formed by deflation of the cuff interferes with intubation, so the selection of the tube can be tricky. Tubes smaller than ID 4.5 are inferior to tubes larger than ID 5.0 in preventing air leakage, and may need a higher cuff pressure to reduce air leakage. For these tubes, minimizing the gap between trachea diameter and cuff size is crucial to reduce air leakage. But tubes with an ID that is larger than 5.0 could be used for much larger trachea without significant air leakage, only if the cuff size is bigger than the ID of the trachea. Further investigations on the design of the cuff, on methods to choose adequate sized tubes, and on reducing air leakage seem to be necessary.
Funding
This work was supported by the 2013 Inje University research grant.