Case Report
Authors:
Dimitri Luz Felipe da Silva*, Fernanda Ometto Pellizari, Maria Letícia Cintra, Elemir Macedo de Souza, Renata Ferreira Magalhães and Andrea Fernandes Eloy da Costa França
*Department of Anesthesiology and Pain medicine, Haeundae Paik Hospital, InjeUniversity, 875, Haeundae-ro, Haeundae-gu, Busan, Korea
Corresponding author
Dimitri Luz Felipe da Silva, Dermatology Division, University of Campinas (UNICAMP), Campinas, São Paulo, Brazil, Tel: +5598 991355216; E-mail: dimitriluzfs@gmail.com
Received Date: 26th May 2018; Accepted Date: 07th July 2018; Published Date: 14th July 2018
Citation
Da Silva DLF, Pellizari FO,Cintra ML, De Souza EM, Magalhães RF, et al. (2018) Brooke-Spiegler Syndrome: Clinical and Histopathological Findings. Enliven: ClinDermatol 4(1): 001.
Copyright
@ 2018 Dr. Dimitri Luz Felipe da Silva. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
A 65 year-old woman with a history of papules and nodules in the face and scalp since childhood, gradually increasing in number and size. The biopsy and histopathological analysis confirmed trichoepitheliomas and cylindromas. Based on histological and clinical findings, the diagnosis of Brooke-Spiegler syndrome, a rare dominantly inherited disorder, was performed.
Case Report
A 65 years-old Hispanic woman presented at our outpatient clinic with a history of multiple, asymptomatic and normochromic papules and nodules in the face since she was six. She received topical treatment with no improvement. One of the skin lesions, presented for 25 years on temporal region, was progressively increasing, especially on the last year. The patient has bilateral hypoacusis, systemic arterial hypertension and dyslipidemia. Her two daughters also have similar skin manifestations.
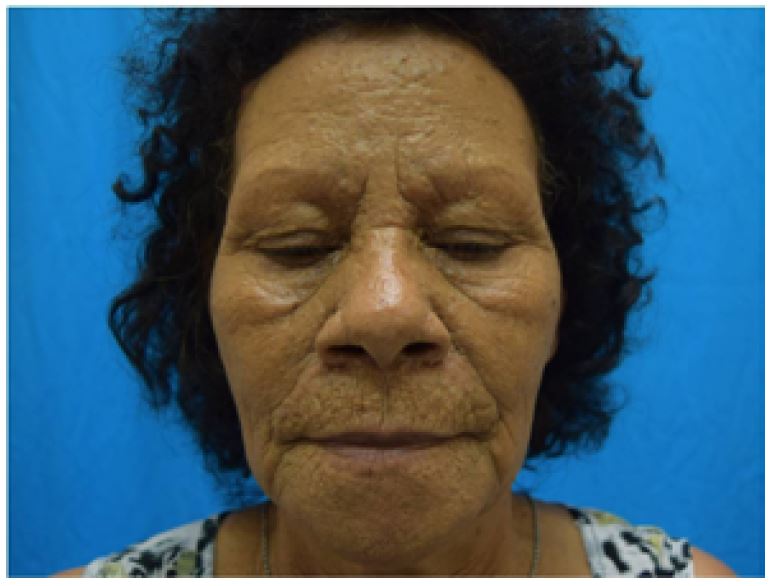
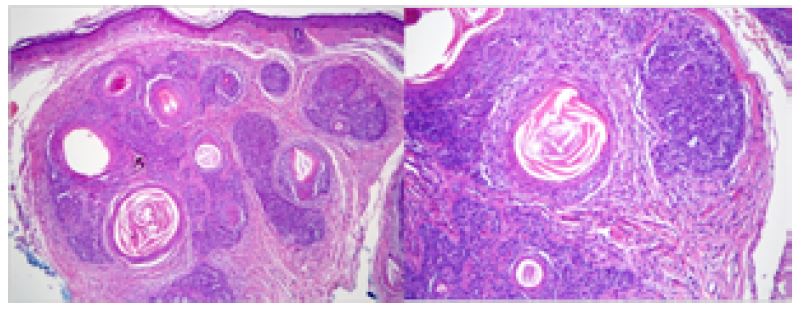
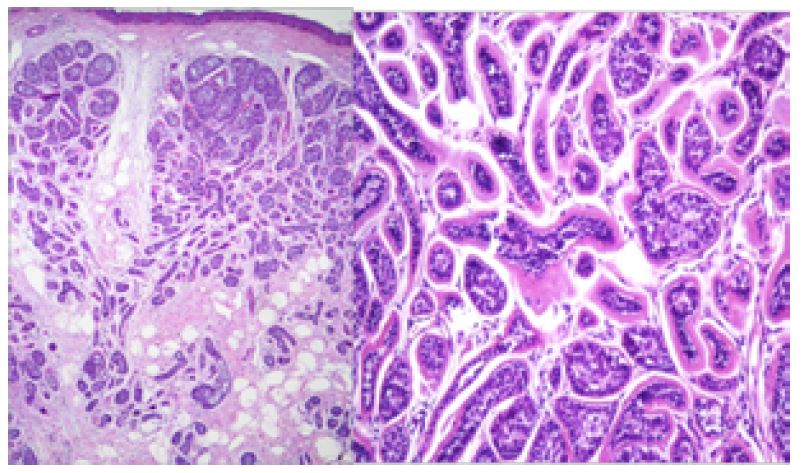
On dermatological exam there were multiple skin-colored and yellow papules on central region of the face and a 2cm light-red plaque on right temporal region (Figures 1 and 2). Histopathological analysis of the nasolabial folds, lesions showed regular islands of basaloid cells with corneal cysts in the dermis, surrounded by adnexal-type stroma, compatible with trichoepithelioma (Figure 3). A biopsy of temporal lesion presented masses of basaloid cells occupying the entire thickness of the dermis, arranged like a jigsaw puzzle, surrounded by an eosinophilic cuticle, consistent with cylindroma (Figure 4). Based on histological and clinical findings, the diagnosis of Brooke-Spiegler syndrome was performed.
Figure 1:Multiple skin-colored and yellow papules on central region of the face
Figure 2:A 2cm light-red plaque on right temporal region
Figure 3:Histopathological analysis of the nasolabial folds
Figure 4:A biopsy of temporal lesion
Discussion
Brooke-Spiegler syndrome (BSS) was named by Weyers in 1993, as a result of the association between multiple trichoepitheliomas and multiple cylindromas, entities describe separately by Henry Brooke and Eduard Spiegler, respectively [1]. It is a rare disorder, with approximately 100 cases reported in literature. BSS is inherited as an autosomal dominant trait, most related to mutations in the tumor suppressor CYLD gene. It is characterized by the gradual appearance of adnexal skin tumors, such as cylindromas, trichoepihteliomas and, occasionally, spiradenomas [2]. Young adults are more affected, with a higher prevalence and severity in women, with no ethnic or racial predilection [3].
The skin appendage neoplasias affect the face (central region and nasolabial folds), neck and scalp, increasing gradually in number and size. Trichoepithelioma is a tumor with follicular differentiation, presenting as numerous rounded and firm papules and nodules, normochromic or yellowish in color, in the facial central region [4]. Solitary trichoepithelioma may simulate basal cell carcinoma, clinically and histologically. Cylindroma is an apocrine differentiation tumor, arising as single or multiple plain erythematous nodules, with telangiectasias on the surface, located in the scalp. The lesions may coalesce and evolve to a final turban appearance. Malignant degeneration of preexisting cylindromas may also occur [5,6].
Patients with BSS are also at risk of developing tumors of the major and minor salivary glands, typically membranous basal cell adenoma. The most important concern about BSS is the aesthetic disfigurement. Neoplastic lesions can be treating by simple surgical excision, electro surgery, cryosurgery, and dermabrasion or laser therapy [7].
This case presents the syndrome findings and reviews some of the histological features in order to spread more about this rare syndrome and the importance of a proper diagnosis and follow-up.
References
- Lavorato F, Miller MD, Obadia DL, Nery NS, Silva RS (2014) Syndrome in Question: Brooke-Spiegler Syndrome. An Bras Dermatol 89: 175-176.
- Szepietowski JC, Wa?sik F, Szybejko?MachajG, BieniekA, Schwartz RA (2001) Brooke–Spiegler syndrome. J European Academy of Dermatology and Venereology 15: 346-349.
- Mataix J, Bañuls J, Botella R, Laredo C, LucasA(2006) Síndrome de Brooke-Spiegler: unaentidadheterogénea. ActasDermosifiliogr 97: 669-672.
- Parente JNT, Schettini APM, Massone C, Parente RT, Schettini RA (2009) Vocêconheceestasíndrome? Síndrome de Brooke-Spiegler. An Bras Dermatol 84: 547-549.
- Jarrett R, Walker L, Bowling J (2009) Dermoscopy of Brooke-Spiegler Syndrome. Arch Dermatol 145: 854.
- Borik L, Heller P, Shrivastava M, KazlouskayaV (2015) Malignant cylindroma in a patient with Brooke Spiegler syndrome. DermatolPract Concept 5: 61-65.
- Nikoletta N, Katalin F, Lajos K, Márta S (2015) Knowledge explosion for monogenic skin diseases. World J Dermatol 4: 44-49.